Neurofeedback improves quality of life, sensory integration, motor skills, movement initiation and balance in Parkinson’s Disease.
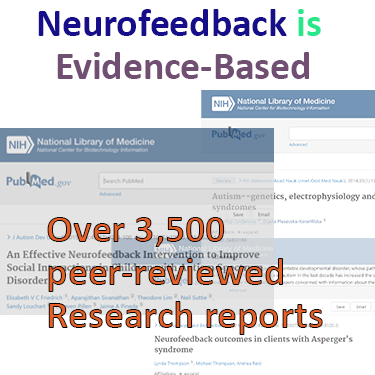
Peer-reviewed research shows the following effects in neurofeedback applications to Parkinson’s Disease:
– improvement in static and dynamic balance
– improved motor symptoms, on a par with other therapies such as rTMS – while being non-invasive and drug-free
– improvement in life quality
– potential to train up speed of movement initiation by 37%
– increased sensory integration in 10-12 sessions
– reduced symptom severity

General (non-PD specific) effects of neurofeedback training include:
– overall increased fine motor skills
– boost behavioural performance and learning
Comorbid mental health issues, such as anxiety, depression, aggression, and mood imbalances can be addressed directly with neurofeedback.
Chronic Pain is another application for neurofeedback, where studies have demonstrated its efficacy.
Subjectively, PD sufferers find neurofeedback training calming, reassuring and report an improved sense of feeling being part of their body.
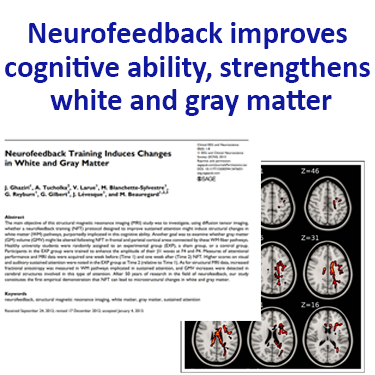
It has recently been shown that neurofeedback training led to cognitive improvements in Multiple Sclerosis (MS) patients, and that this corresponded to improved functional connectivity in key motor and salience networks. Increased fractional anisotropy (FA) was observed, which correlated with cognitive improvement.
MS is a neurodegenerative condition that adversely affects axonal myelination. FA is among other a measure of myelination, so the result that neurofeedback can make positive changes in this condition is very encouraging.
A study with sufferers of Huntington’s Disease, another neurodegenerative condition, showed that cognitive and motor skills improved and that these changes related to improved functional connectivity in key brain regions, again a conclusion that neuroplasticity can be induced despite the presence of neurodegeneration.
Research on audio-visual hallucinations in Schizophrenia patients have found that Neurofeedback training can produce significant results in reducing treatment resistant auditory verbal hallucinations. In 30% of cases antipsychotic medication has little or no effect
Researcher Katherine Fletcher (PhD) of Parkinson’s UK asserts that:
“The idea of Neurofeedback is very interesting and the evidence [above] shows great potential. Larger studies would be needed to fully understand the potential and safety of this method for people with Parkinson’s before we could share it with our community.”
Research funded by Parkinson’s UK regarding hallucinations is currently focused on CBD and anti-sickness pills. Neurofeedback training is drug-free and non-invasive.