Neurofeedback for Anxiety
Quick Navigation
Anxiety clouds our perception and curtails a positive outlook.
Left untreated, a negative feedback loop can ensue: We lose synchrony with our environment, resulting in reduced drive, motivation, activity, interaction, recuperation (sleep) and functionality. Physical manifestations ensue, and we enter a negative feedback loop.
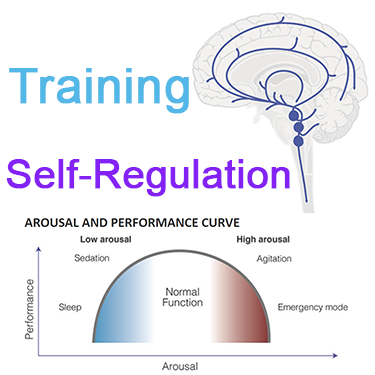
Anxiety is a result of inefficient sensory processing. This leads to dysregulation in our body’s reticular activating system, responsible for physiological arousal regulation, and can have debilitating manifestations such as panic attacks.
As such, it starts in the head, though its manifestations can quickly become physical. Pain perception has neural correlates. With a Kaiser Neuromap we can identify dysrhythmia of relevant brain areas, and then train these with neurofeedback.
We take a holistic approach – as well as training brain areas responsible for arousal, mood and vigilance, we restore focus, drive and motivation, thus restoring self-confidence in a multi-faceted way.
With a Kaiser Neuromap, we can assess vulnerabilities and treat these with neurofeedback in a non-invasive, enjoyable and medication-free way.

There are many manifestations of anxiety, including social anxiety, panic attacks, excess body awareness (body dysmorphia), emotional hypersensitivity, fears and phobias. Autistic children generally present with a variety of these, all contributing towards an energy-consuming heightened state of vigilance. Stress and defensive behaviour results.
Neurofeedback is an established, evidence-based treatment for anxiety.
It was found that neurofeedback training for anxiety and depression “results in enduring improvements approximately 80% of the time”
Confidence and social integration tend to improve accordingly, resulting in a positive feedback loop that helps shape new trajectories.
A brain map will reveal overactivity of brain areas responsible for monitoring consequences of actions (timidity, general fright and reticence); watching out for an abuser (bully); body and face awareness; and excessive self-monitoring. This helps us understand the potential presence of real threats and fear factors. We can also detect possible tendencies to develop unhealthy body awareness. Neurofeedback training lets us address this issues.
Various Forms of Anxiety
There are multiple types of anxiety, each correlating with one or more brain areas being dysrhythmic:
Sensory overload: our brain interprets all sensory stimulus as directed to ourselves. We lose the ability to discern what is directed at us, and which matters or interactions are of no concern to us. This sets us up for panic attacks and ultimately psychosis. It also means we become singular in our perspective, unable to take on other points of view
Loss of narrative: Our episodic understanding of the situation, how we got there and what happens next, is impaired, and we are unsure of where we are and where we’re going. This hyperactivates our amygdala, and the sensation is highly emotional
Auditory sensitivity: we become prone to overly interpreting the emotional content of words and sounds, creating an air of prickliness and pushing people away without knowing it
Social anxiety: misunderstanding social complexities, social emotions and dynamics in a situation with others
Hypervigilance: as a result of avoiding a bully or abuser
Activation: Our ARAS is responsible for setting the right level of physiological arousal, or wakefulness, for the situation, and to remain stable there. When this is on overdrive, we are pushed further into fight-or-flight mode than necessary, thus heightening sensory sensitivity. Panic attacks are an extreme manifestation. Our ability to calm down quickly is reduced.
Trauma: an inability to self-nurture – creating an emotional safe-space around us – and self-soothe – being able to talk ourselves down rationally from a situation, thus resulting in mood instability. This can also manifest in dissociation and heightened pain perception. We ruminate about the past and worry about the future, instead of being able to enjoy the present.
Intrusive thoughts: Self-criticism overshadows motivation and confidence, and we become self-aware and distracted by negative thoughts and feelings. Some use acquired habits to distract from this. Others become attached to the reward circuitry triggered, and sustained by feeding obstructive, self-deprecating thought content. Our confidence, motivation and social interaction suffer as a result.
Neurofeedback and POTS, Anxiety
Postural Tachycardia Syndrome (PoTS) was first described in the 1940s, refined in 1993 and finally received a specific diagnostic code in October 2022. It is characterised by exercise intolerance and near syncope upon standing upright, elevated pulse (tachycardia) by 30-40bpm within 10 minutes of standing up, fatigue, anxiety and light-headedness. Often misdiagnosed as chronic anxiety or panic disorder, the group of symptoms comprised by PoTS has a biomarker and increasingly considered an autoimmune disorder, rather than only autonomic nervous system dysfunction. Specifically, increased levels of cytokines and chemokines characteristic of an innate immune condition were found, similar to autoimmune diseases like multiple sclerosis, psoriasis, type-1 diabetes, rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
The condition affects females five times more frequently than males, mainly between 15-25 years of age, with over one million affected in the US alone. PoTS symptoms can persist for years, though half of patients find that orthostatic symptoms and functional impairment subside within five years, and of thost most within 1-2 years. It is estimated that 2-14% of Covid sufferers go on to develop PoTS, while 30% of long Covid patients, especially women, meet the diagnostic criteria.
A client presenting with PoTS like symptoms, recovered within three months of starting neurofeedback training, to the extent that the tachycardia was fully under control and anxieties had subsided substantially. Clinical studies will have to prove correlation. Notably, physical symptoms became manageable, from being previously incapacitating, in a relatively short period of time. This result is encouraging, especially with regard to the speed and extent of recovery, and neurofeedback has been shown to be effective for anxiety. Also, in this person, other neurological issues could be detected with qEEG.
Neurofeedback is a Proven Treatment for Anxiety
Evidence: Neurofeedback for Anxiety
The effectiveness of neurofeedback training for anxiety was first recorded four decades ago in 1978. Since then, there have been over 120 peer-reviewed research papers published on neurofeedback and anxiety. Academic interest in this application of neurofeedback has picked up notably during the last three years.
Dr. Corydon Hammond finds in his 2005 paper, “Neurofeedback Treatment of Depression and Anxiety” that neurofeedback training results in “enduring improvements approximately 80% of the time”, with most perceiving a difference after between three and six sessions; a “very significant improvement” after 10-12 sessions, and more so after over 20 sessions.
Improving emotional regulation with neurofeedback represents a “novel intervention to control anxiety”. Just a single session resulted in a statistically significant improvement in anxiety.
Contamination anxiety was improved in a lasting way in this study .
Twenty sessions of neurofeedback training led to a significant improvement in sleep, anxiety and depression evaluations. The same disorders plus inattention showed significant improvements when conducting ten or more sessions in a naturalistic setting. Anxiety was reduced in Canadian Aboriginals during seven days of two hour training. Fifteen sessions reduced GAD symptoms.
Neurofeedback improved depressive symptoms in Major Depressive Disorder (MDD) patients, with significant decrease in anxiety and clinical illness severity noted as a result of the training. Cognitive depression was reduced here. Anhedonia and comorbid anxiety in MDD where also improved in this recent study. Increased happiness ratings and decrease in anxiety was documented with related increased activity in specific brain areas.
Post-operative depression and anxiety, pain, difficulties sleeping and attention and memory problems were resolved in 20 neurofeedback sessions. The 45-year old female was able to return to work subsequently. Postcancer cognitive impairment (PCCI) sufferers (a substantial subset of breast cancer survivors) found strongly significant reduction in anxiety, as well as somatisation and depression, after twenty neurofeedback sessions. Anxiety, as well as depression and tinnitus were greatly reduced during stroke rehabilitation, plus improvement in speech fluency, word finding, balance and coordination, attention and concentration.
Ten neurofeedback sessions improved symptoms of pain and fatigue, anxiety and depression in fybromyalgia patients. Neurofeedback was also found to reach maximum effect within four weeks.
Multiple Sclerosis sufferers saw depression, fatigue and anxiety reduced, and the results were maintained at a 2-month follow-up.
Alpha Theta neurofeedback training reduced anxiety in competitive ballroom dancers, as well as increasing cognitive creativity.
Neurofeedback provided benefit to high functioning ASD with regard to anxiety.
Alcohol Dependence Syndrome patients found a significant reduction in cognitive deficits, anxiety and depression; noticeable improvement in memory and neurological functioning, and significant reduction in alcohol intake on follow-up. Impulsivity, anxiety and depression were improved in long-term abstinent delinquents. Sharp reductions in self-assessed depression were found in alcoholic outpatients, as well as reduction in anxiety, after twenty Alpha-Theta sessions.
The physical basis of how neurofeedback training can be applied to reduce maladaptive rumination and anxiety was confirmed here.
Case Study: Anxiety, Panic Attacks and Depression
Camilla had been diagnosed with anxiety, panic attacks, associated insomnia and mild depression. She was prescribed two anti-depressants – Mirtazapine and and SSRI – which she was able to reduce to a minimum dose over time. During the last three years however, she had six relapses, each following a similar pattern: Stress (emotional and work-related) and fatigue precipitated intrusive thoughts and worries, setting off a familiar path of insomnia; consequently higher anxiety, increased stress levels leading to panic attacks and depressive symptoms. The first few episodes were stabilised by resuming Mirtazapine, which helped restore sleep. The subsequent ones however failed to respond, taking months to stabilise sleep and reduce anxiety, which involved having to take time off work. In addition, she began to have somatisations, beginning in the spine and ultimately reaching her face. Migraines began to reappear when she became excessively tired.
Guided by a brain map, we began doing neurofeedback training twice a week. Camilla’s sleep became sound after the second session – “I feel pleasantly knocked out” – and she decided to reduce her Mirtazapine dose gradually in accordance with her prescribing GP. After eight sessions (four weeks) she was on the lowest dose, and even this left her feeling very groggy in the morning. Camilla had regained confidence in her ability to fall asleep, and stopped using Mirtazapine completely. Her anxiety levels were at their lowest, and she had began to work again, leaving a corporate environment to work with children in a mental health setting – a stressful yet engaging and meaningful activity. Her motivation had reached new levels, and she felt stable and confident, which showed in her stance and demeanour.
Ten sessions of neurofeedback training (each two hours) were sufficient to stabilise Camilla, restore her ability to sleep, and the confidence therein, as well as improving sense of self-worth, focus and motivation. She has not felt the need to use Mirtazapine again since.
Three months later, Camilla reports a major improvement in how she is able to set boundaries, both at work and in her personal life, and not neglecting her own well-being.
Brain Maps and Personalised Brain Training Explained
Personalised Brain Training with Neurofeedback
Neurofeedback lets us train dysrythmic brain areas. With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, short and instantaneously.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the movie; the training process is passive in this sense.
The drop in volume is subtle, so we continue to understand the flow of the movie. No current or electrical stimulation is fed to the brain; sensors simply read brainwaves and the feedback is purely audio-visual.
Neurofeedback trains our Pre-Conscious Mind
Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
This equips us with the ability to live in the moment and attain our potential (if we have to resort to conscious control, we are not living in the moment).
We take a holistic approach to healthy brain self-regulation, rather than categorisation or diagnosis.
Personalised Brain Training is an advanced qEEG brain map-based approach to neurofeedback training developed by the founders of the field. Taking Othmer Method / ILF training methods further, it employs Default Network Training protocols as developed by David Kaiser.
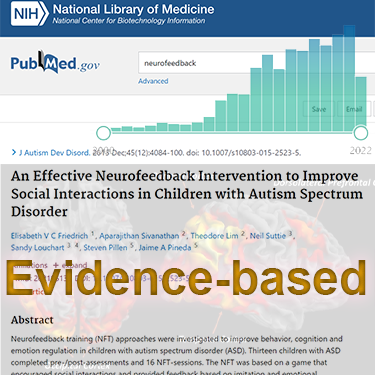
Neurofeedback is Evidence-based
Neurofeedback training is an evidence-based complementary therapy. Its efficacy was first demonstrated some 50 years ago, and with advances in technology, training protocols have become more efficient and the feedback method – watching movies – thoroughly enjoyable.
Neurofeedback is evidence-based. It’s first application was discovered in 1971 when it was used to resolve intractable epilepsy.
There are over 2,000 peer-reviewed research reports on PubMed demonstrating efficacy across a number of pathologies.
In the US, it is an accepted complementary treatment for many challenges.
Neurofeedback: Two Approaches, Othmer Method and qEEG Brain Map-based Personalised Brain Training
With the Othmer Method of neurofeedback training, we can achieve calming and improved emotional self-regulation.
Brain Map-based Personalised Brain Training lets us target specific brain areas. There are many sources of anxiety. With a qEEG brain map we can see dysrhythmia in specific areas of the cortex that may contribute to anxiety. Personalised Brain Training then lets us train these areas as part of a holistic approach to optimal cortical integration.
The Othmer Method for Anxiety: Mental Calming and Trauma Resolution
First, neurofeedback works on emotional and physical calming. The effects are often felt within the first few sessions; further training allows these to become permanent.
This is done with ILF training using the Othmer Method, whereby the parts of the brain responsible for physical symptoms, for core emotions such as fear and anger, hyper-vigilance and paranoia, for self-control and conscious obsessive thoughts are trained.
Often, anxiety is rooted in some form of Trauma.
Once sufficient calming is achieved, Alpha Theta training is used to address underlying trauma, issues or memories which haven’t been digested, and enable the brain to process these, consciously and subconsciously. Importantly, Neurofeedback training aims to resolve trauma subconsciously, without having to relive the trauma. Alpha-Theta Training, a very relaxing protocol, allows our brain to reach deep states during which it is able to separate the event from the emotions attached to it, and store these memories and associations in a safer place.
Adding Synchrony training can further soothe, improve memory and concentration, and generally restore a healthy sense of self-worth and connectedness with our environment.
Anxiety and Physiological Arousal – Improving Brain Self-Regulation with the Othmer Neurofeedback Method
Each person has their individual arousal and performance curve. We move up and down this curve over the course of the day as we are confronted with situations.
At the high end, extreme arousal constitutes a hyper-vigilant state mentally, and the physical symptoms to match, e.g. higher heart rate, blood pressure, sensory alertness and readiness to respond. This is useful in emergencies -“fight or flight” – but ignores necessary rest and recuperation, as well as an awareness of the future and resultant needs for foresight and preparation; it also places unsustainable stress on the body and consequently is not a state that should one should be in continuously. At the other extreme, a low arousal state is essential for good rest and sleep, but is not suited to the range of demands in our daily routine, which can include times of high levels of alertness, varying degrees of physical preparedness, repetitive tasks with different concentration requirements, and all kinds of emotional states paired with their concomitant physiology.
The ability to shift arousal state to the requisite level for the situation at hand is what is meant by good self-regulation of the brain. It is this quality that neurofeedback training seeks to improve.
Alpha Theta Brainwave Training for Unresolved Trauma
The root cause of anxiety can be an unprocessed experience, or possibly a trauma one isn’t even conscious of anymore. A variation of neurofeedback training, Alpha Theta, aims to induce a deep state of relaxation during which it is possible to safely digest such issues and enable them to enter the long term memory, free of the feared emotional association. From clinical experience, the processing of emotions and memories appears to happen particularly when we are crossing from the meditative Alpha state into dream-intense Theta; during Alpha Theta training, the brain is given information as to which state it is in – the music changes, basically, though we add other auditory components such as chimes, gongs and binaural beats. We are not forcing the brain to do anything, other than to relax by being in a quiet, comfortable setting wearing eyeshades and headphones. In a twenty to thirty minute session, the brain shifts between Alpha and Theta dominant states repeatedly, and processing of experiences happens at subconscious and conscious level.
Alpha Theta training can be very deep, and requires a certain calmness of mind in order to be tolerated – it is an eyes-closed exercise during which unwanted experiences may surface, though many are dealt with by the unconsious mind. Digesting experiences means separating the emotion from the event and enabling the brain to file the entire trauma differently, in a form that is accessible yet not tainted with negative or adverse feelings and associations. During Alpha Theta training, this can occur without reliving the event consciously, which can be highly efficient both in terms of time and effort. We would generally add this training after at least ten ILF Othmer Method sessions aimed at calming, though readiness can vary.
Synchrony Training for Stress & Anxiety
Infra-Low Synchrony training engages the Default Mode Network directly, and we have seen many cases where this has led to an improved sense of self-worth and a strong feeling of connectedness to our environment where this was lacking before, obscured by chronic stress and symptoms of anxiety.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
The Process Explained
Step 1: Brain Map
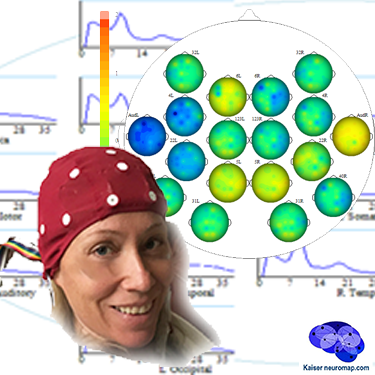
A qEEG recording takes about 45minutes for a 20 minute recording.
A cap with 19 sensors is is fitted to our head and gels inserted to ensure connectivity. The sensors only read – there is a tiny voltage on the surface of our head that these pick up. The gels are easily washed out later. This is also the last time we wear the cap (until a remap after ten sessions); training is done with single sensors.
We analyse the data with Kaiser Neuromap software which gives us a unique view into character traits and vulnerabilities.
Findings are presented in a separate one-hour conversation where we discuss the key elements.
Step 2: Neurofeedback
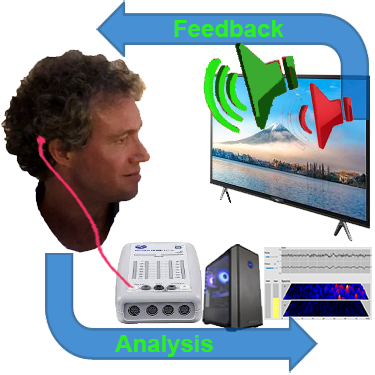
We use a movie of choice as the feedback mechanism – our conscious mind engages with the film, and feedback is delivered by small changes in volume or picture size.
Our pre-conscious mind adapts its behaviour to preserve the more comfortable volume and picture size, and learning occurs.
Volume changes are slight, not stop-start, and the process is enjoyable.
Key is that we are interested in the movie – our conscious mind is engaged with the content, which forms the reward, and our preconscious mind – without our conscious effort – changes its behaviour in response to the feedback.
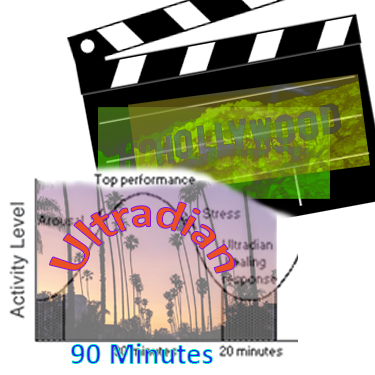
A two hour training session allows us to do 90-110 minutes of neurofeedback training during which we can work on various brain sites.
This captures an entire ultradian rhythm cycle and corresponds to the approximate duration of feature film movies.
We can start with shorter sessions as appropriate, mainly with children.
Ideally, we do two or more sessions per week to start with.
We would expect to see responsiveness within the first few sessions and remap after twenty hours or about ten sessions.
Generally, we would expect to doing twenty sessions over two months, though this can vary substantially.
We can also accommodate intensives, where we do two sessions per day over a number of days, and have had good results with these.