Neurofeedback for Clinicians
Quick Navigation
Neurofeedback - A Complementary Therapy
Daniel Webster works closely with psychiatrists, psychologists, social workers and other mental health professionals, both in private practice and in the NHS. Observing and tracking client progress is best done in collaboration with others, and helps shape optimal outcomes.
A brain map provides a complementary perspective on a person’s vulnerabilities, strengths and development, including character insights that might be masked by the individual. Neurofeedback training improves the person’s grounding, sense of self, interoception and communication, making it an ideal complement for psychotherapy and other treatments.
Effects of medication can be tracked with remaps, and we have effectively managed clients off medication in close collaboration with the prescribing entity where this was no longer productive. The medical intervention can thus be applied with a view to eventual cessation and transition. In many clients we have found that stimulant or depressant medication has undesirable effects, such as various forms of anxiety and fatigue, and neurofeedback has helped them reduce and eliminate this.
We can track and benchmark physical development properties of the brain, which is particularly useful in children. There are (non-specifid) neuromarkers for various degenerative conditions, including Alzheimer’s, concussion / mTBI. We can disaggregate more general pathologies such as anxiety, trauma and depression into more granular components with neural correlates. This improves our understanding of the client, the treatment plan, outcome and our own sense of achievement that is important in sustaining a mental health career.
Personalised Brain Training is a complementary therapy method that can help Psychiatrists, Psychologists, and other mental health professionals improve their results with clients.
As clinicians, we are constantly looking to improve
– our understanding of the client’s needs and potential
– therapy approaches to help the client, quickly and effective
– our sense of achievement and ability to consistently give our best.

Personalised Brain Training, a form of qEEG-brain map based neurofeedback training, can help us in many ways:
– brain maps provide diagnostic support, highlighting vulnerabilities with respect to behaviour, sensory integration, development and more
– they show strengths and opportunities with a view to being able to measurably improve brain function, mental health and overall performance
– social behaviour characteristics can be seen and interpreted, providing another ‘window’ into masked attributes
– neurofeedback is an evidence-based complementary therapy, demonstrated for many pathologies, and is shown to aid in physical development, rehabilitation and in neurodegenerative conditions
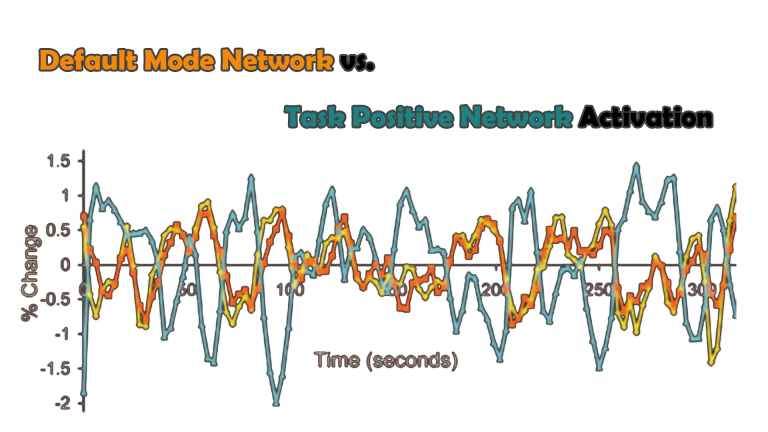
– Default Network Training is the most advanced form of personalised neurofeedback training; it is also enjoyable as it involves watching movies; the process is uninterrupted as feedback is given by slight temporary changes in volume; and it requires only minimal dialogue
– results are transformative and mostly achieved within 10-20 sessions, or 3-6 months, reshaping developmental trajectories and providing a basis for psychotherapeutic interventions and coaching
– we see clients progress, organically and unmedicated, (re-)gaining a healthy sense of self, interacting socially, yielding anxiety to hope and positivity, and achieving their full potential
– changes are visible on a brain map (we remap every ~10 sessions), and observable; clients understand their progress, develop better interoception and ability to communicate their state, and are thus empowered throughout monitoring
– the client relationship becomes energising.
The Brain as the Source of Mental Health
Our brain governs our interaction with our environment, manages our reactions and anticipations, harbours our dreams and visions, and digests our experiences.
Ideally, as mental health professionals, we would like to be looking into the organ that drives our behaviour.
(Scroll down on mobile)
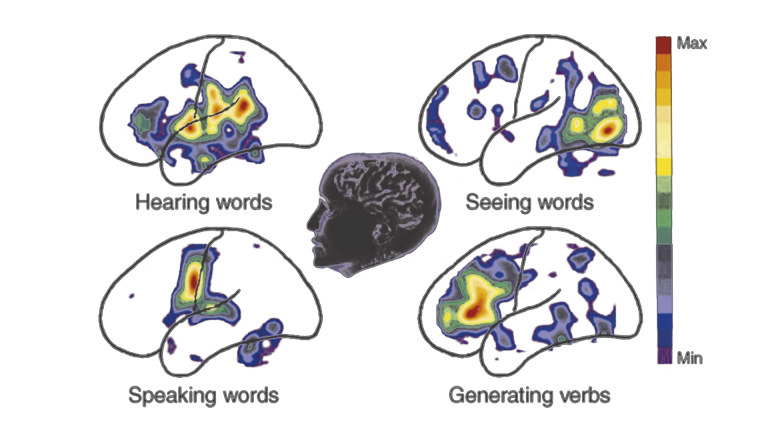
Sensory processing is one of the most basic functions of our cortex. Relayed throught the thalamus (except smell), sensory input is delivered to specific cortical regions that interpret the neuronal signals. Multi-modal association areas help put together a complete picture of our environment, integrating processed information from various sensory association areas with regard to our position and relevant experiences.
We start generating a model of our perspective and story – autobiographical self. Our model of our environment expands to other people, whom we can attribute agency to, learn to predict and correct, and create relationships with.
In autism and schizophrenia, this is a particular issue. There are many more sub-clinical variants that can exhibit particular, individual weaknesses with regard to the above processes.

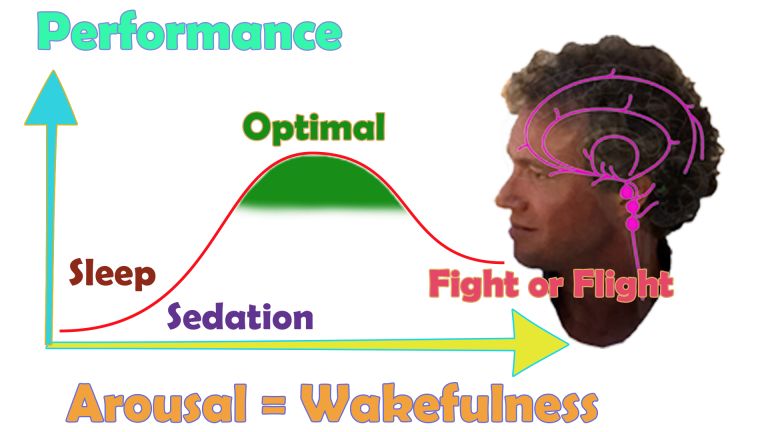
Our brain initiates the steps to regulate our physiological arousal, setting the right level of activation for the task or situation at hand; maintaining a stable level; and adjusting this flexibly as needed.
It regulates our autonomous nervous system, setting the physiological tone of arousal for our interaction with the environment: based on experience and anticipation, our heart rate, breathing, blood pressure, muscle tone, waking hours, alertness and more. This in turn influences our mood, productivity and social interactions.
There are multiple reward and pain pathways, affecting motivation and decision-making. Sleep is a complex process and our brain manages the transition between various phases that help us physically recuperate and consolidate learned behaviour while maintaining bodily homeostasis.
Unlike the reptilian brain, our cortex permits us to repurpose primal urges into pro-social, collaborative and civilisation-building behaviour. The cortex is an expensive organ to run, consuming 20% of our energy while making up only 2% of our body mass. Its efficient use is an important part of our evolution, and some key advantages is provides are the ability to interact socially, making friends and alliances; and to anticipate and plan for the future.
Fundamentally, our brain is able to form models of our environment, including people, predicting on the basis of past experience, and checking prediction errors by updating sensory information, thereby improving its next anticipation among probable outcomes. This gives us the ability to empathise, track motion, sequence events and plan, create and enjoy music, and respond flexibly to changing situations and unanticipated outcomes.

From imagining actions, planning their execution, prompting motor skills, monitoring and correcting, there are many specific brain areas involved that work together with our sensory integration and decision making.
Speech and language use these resources, and we use verbal and non-verbal skills to communicate and synchronise with others.
Self-reflective thought, memories and imagination activate our Default Mode Network, a set of key brain areas that constitute our neural definition of self. Our brain oscillates activation of these nodes with areas of the Task Positive Network, and a clean, counter-(/anti-)cyclical activation pattern is important for mental health – flexibility.
Within the Default Mode Network, there are brain areas that are responsible for our ability to self-nurture and self-soothe, that is, our ability to create emotional safety and also rationally talk ourselves down from a situation. Trauma, its memory and how this shapes our future behaviour, is anchored in the brain.
There are specific brain areas that deal with our personal and social boundaries. When these are weak, we can become excessively recruitable, obstinate or invasive. Our social boundaries are another person’s personal boundaries, and our cortex manages this interplay.
Social rules, turn-taking and monitoring of consequences is an additional process governed by our executive brain areas.
Importantly, these are pre-conscious processes, and to effectively live in the moment, we would like for these areas to work together efficiently. Overriding impulses with conscious control introduces a delay that interrupts our synchrony with our surroundings, and we no longer live in the moment.

Our brain has over 40 distinct functional areas, delineated by their cytoarchitecture (grey matter layer attributes), by Korbinian Brodmann in 1909. There are almost 200 new research reports per year dedicated to the exploration of their individual functions, usually by way of psychological experiments monitored by fMRI. This provides us with bio- or neuromarkers for particular behaviour patterns that are characteristic of certain pathologies. It’s also a more granular way of exploring the various contributors to a person’s maladaptation.
A Kaiser Neuromap is a particular analysis of qEEG information. We are looking for persistent traits, rather than state-specific fluctuations, and how these relationships compare with healthy controls. This brain map shows us the level of connectivity between functional Brodmann areas, as well as indicating hypometabolism. It is not a diagnosis, and shows vulnerabilities as non-specific, meaning they are necessary, but not sufficient conditions for a pathology.
We can also see many tendencies that might only have sub-clinical manifestations. A brain map helps us understand character attributes and behavioural tendencies that are masked by the individual.

Personalised Brain Training
Personalised Brain Training is neurofeedback training using the most advanced protocols, on the basis of a qEEG brain map. Training is enjoyable and results are measurable.
(Scroll down on mobile)
We do a twenty-minute qEEG recording, which takes about forty minutes including setup. Analysing this shows us which Brodmann areas are dysrythmic, that is, which cortical areas are not contributing sufficiently and are thus prone to ‘immature’ or limbic performance.
For example, a brain area that processes spatial awareness and imagined actions can show up as being immature. This indicates that the person is vulnerable to distractibility. Similarly, an area processing social complexity can be dysrythmic. As a result, the person is prone to social anxiety. There are neuromarkers for a wide range of behavioural tendencies, showing vulnerabilities – necessary, but not sufficient conditions.
Analysing prevalent frequency distributions also indicates physical maturity of the brain, which is particularly relevant in children.
A brain map can help a psychiatrist, psychologist or other mental health professional gain an alternate understanding of a client’s situation, based on physiological data (qEEG).

The idea that certain brainwave patterns are linked to a state of mind was spawned in 1923 when Dr. Hans Berger observed alpha spindles in the EEG of a person at rest / with their eyes closed. The developing field of biofeedback began extending its input to EEG, and by 1972 Dr. Barry Sterman effectively established neurofeedback as a new discipline. Sterman was able to train cats to increase their SMR (sensori-motor rhythm), which resulted in increased seizure resistance. This finding was replicated in humans, a theory being that such operant conditioning can increase GABA-receptors in the brain.
Several technological advances make neurofeedback today an enjoyable process, where our conscious mind is focussed on a reward, such as watching a movie, while the feedback is subtle and built into the reward modality through slight, temporal volume changes. The training protocols devised by Dr. David Kaiser, applied to findings from the qEEG analysis software he developed with Dr. Barry Sterman, are the most advanced in the industry. Based on a brain map, we do two-hour sessions, corresponding to an ultradian wakefulness cycle, and find most achieve transformative effects within 10-20 sessions.
Improvements, changes in functional connectivity and cortical maturity, are visible on a remap, and correspond to the client’s perceived changes.
The Science of Compassion

Compassion is a core component of effective care-giving. To be sustainable, the client relationship has to become reciprocal in that the care-giver continues to derive satisfaction from their work. The Science of Compassion formalises these needs and provides a framework to improving clinical experiences for everyone.
(Scroll down on mobile)
Modern researchers define compassion as having 4 components:
(Jinpa, 2012; Jazaieri et al., 2016)
• 1. Noticing another’s suffering (cognitive/attentional component)
• 2. Empathically feeling the other person’s pain (affective component)
• 3. Wishing or desiring to see relief of that suffering (intentional component)
• 4. Responding or acting to help ease or alleviate that suffering (motivational component)
Compassion Satisfaction is defined as:
• A positive sentiment the provider experiences when able to empathetically connect and feel a sense of achievement in the careproviding process.
• Increased sense of self-efficacy and fulfilment in helping work
• Invigorated in the work and energized further to contribute to helping people who need care.
(Stamm, 2002; Stamm, 2010; Slatten et al., 2011; Zeidner & Hadar, 2014)
Dr. Dominic Vachon of the Ruth M. Hillebrand Center for Compassionate Care in Medicine, University of Notre Dame, explains.
Other universities with research centres dedicated to the Science of Compassion include:
– University of California, San Diego (UCSD)
and other institutions.
Dr. Dominic Vachon of the Ruth M. Hillebrand Center for Compassionate Care in Medicine, University of Notre Dame, explains.
Other universities with research centres dedicated to the Science of Compassion include:
– University of California, San Diego (UCSD)
and other institutions.
As mental health and neurodiversity are gaining broader acceptance, demand for effective therapies is set to grow strongly and steadily. Private mental health services will increase their share from the currently ten percent of the already growing total expenditure. About half of mental disorders start developing before the age of fourteen. Mental health services will improve their focus on children and adolescents as the industry becomes more efficient and results-focussed.
Brain Maps and Personalised Brain Training Explained
Personalised Brain Training with Neurofeedback
Neurofeedback lets us train dysrythmic brain areas. With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, short and instantaneously.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the movie; the training process is passive in this sense.
The drop in volume is subtle, so we continue to understand the flow of the movie. No current or electrical stimulation is fed to the brain; sensors simply read brainwaves and the feedback is purely audio-visual.
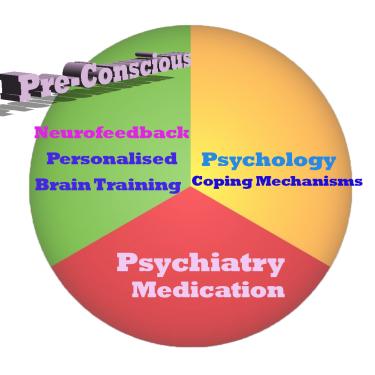
Neurofeedback trains our Pre-Conscious Mind
Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
This equips us with the ability to live in the moment and attain our potential (if we have to resort to conscious control, we are not living in the moment).
We take a holistic approach to healthy brain self-regulation, rather than categorisation or diagnosis.
Personalised Brain Training is an advanced qEEG brain map-based approach to neurofeedback training developed by the founders of the field. Taking Othmer Method / ILF training methods further, it employs Default Network Training protocols as developed by David Kaiser.
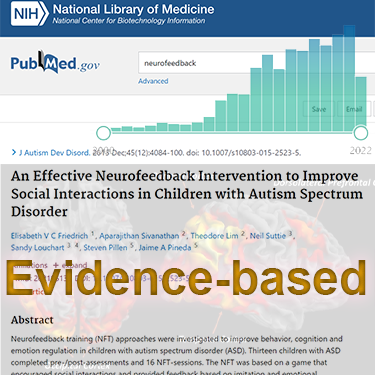
Neurofeedback is Evidence-based
Neurofeedback training is an evidence-based complementary therapy. Its efficacy was first demonstrated some 50 years ago, and with advances in technology, training protocols have become more efficient and the feedback method – watching movies – thoroughly enjoyable.
Neurofeedback is evidence-based. It’s first application was discovered in 1971 when it was used to resolve intractable epilepsy.
There are over 2,000 peer-reviewed research reports on PubMed demonstrating efficacy across a number of pathologies.
In the US, it is an accepted complementary treatment for many challenges.
Neurofeedback Improves Symptoms in Autism
Autism is a spectrum disorder characterised by social integration issues and developmental delays that can be both physical and emotional. With a Kaiser Neuromap we can identify individual weaknesses, and train these with Personalised Brain Training in a non-invasive, medication-free manner. Improvements are evidence-based and impressive.
In particular, we can identify and train vulnerabilities to behaviour patterns:
– sensory integration: sensitivity to sound, light, taste and touch, motor coordination; balance, bodily and spatial awareness
– social functioning: social cues, taking turns, Theory of Mind, collaboration with others, social rules and boundaries
– self-regulation: mood and impulse control, impulsive aggression and rage, fear and anxieties, ability to self-soothe / self-nurture, repetitive restrictive behaviour
The result is a calmer, better integrated child, who can maximise their true social and productive potential.
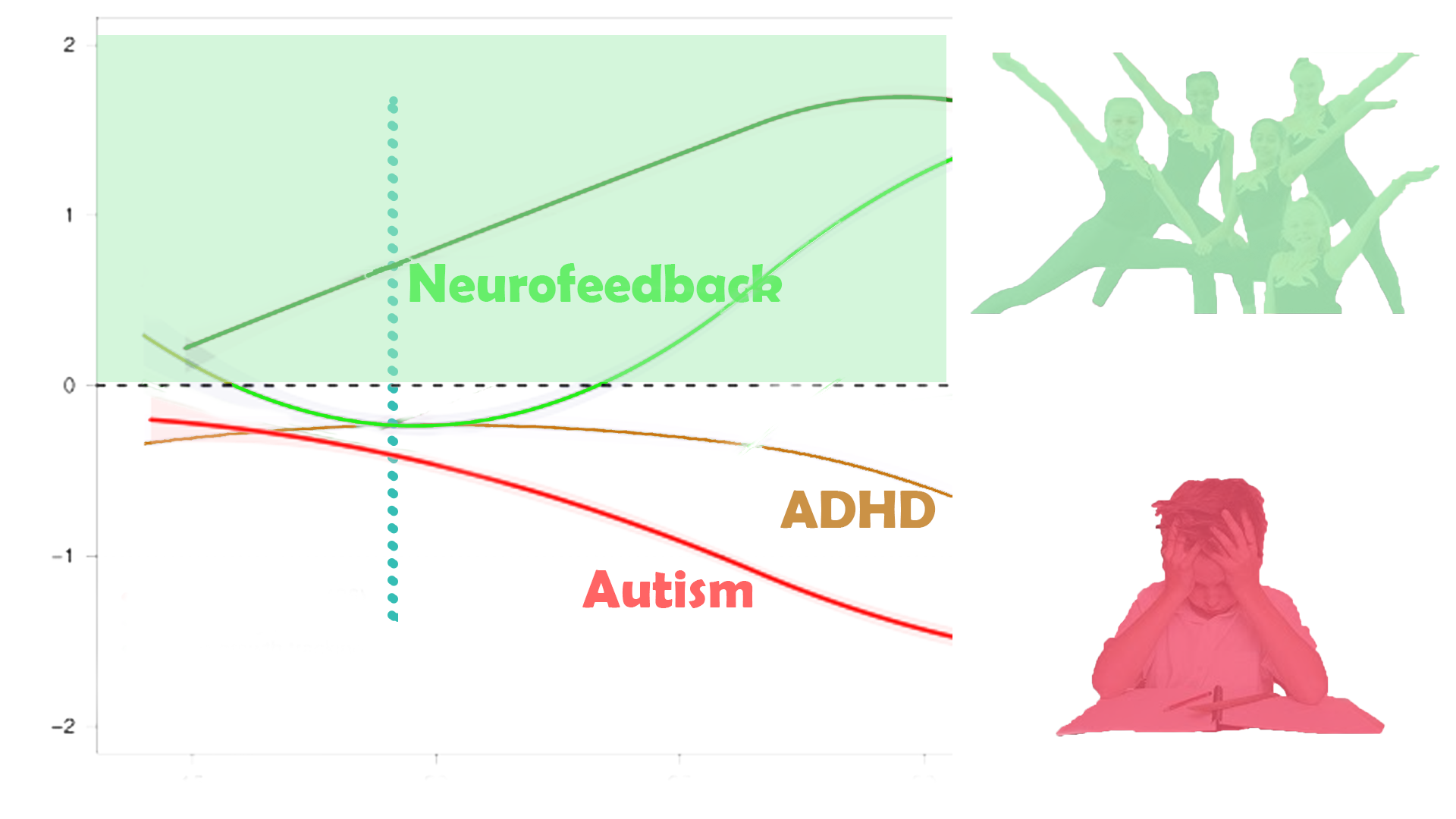
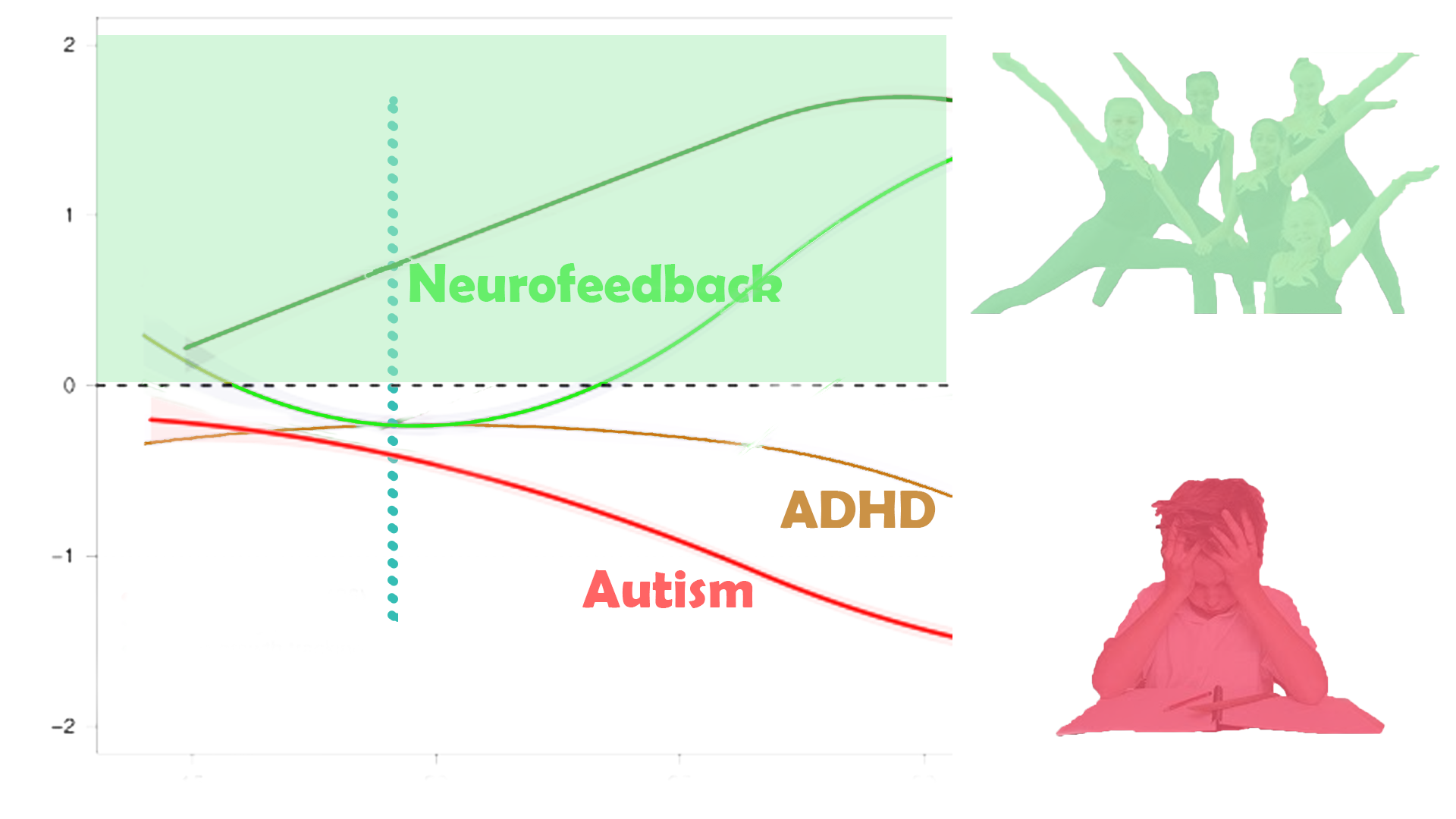
Changing Development Trajectories
With Personalised Brain Training, we can change developmental trajectories.
Improved sensory integration, social functioning and self-regulation helps unfold potential and the ability to live life to the fullest possible.
Future care efforts and costs can often be substantially reduced as a result. The average lifetime cost of supporting an autistic person is estimated at $2million+. In comparison, neurofeedback training, while cost-intensive, is a fraction of this.
Enabling greater talent expression can lead to improved earnings potential and financial self-sufficiency. These ‘dividends’ materialise over time, and their present value can exceed the investment made in Personalised Brain Training at an earlier stage by multiples.
Neurofeedback training is non-invasive and medication-free, and this organic treatment approach respects the individual’s choices.
Neurofeedback and Autism
A brain map lets us look into our brain – how the different parts communicate with eath other. With neurofeedback, we can train optimal integration.
The following tabs describe how Personalised Brain Training can help resolve many mental health issues in a holistic, non-invasive and medication-free manner.
(Scroll down on mobile)
"Anna was definitely a lot calmer, didn't 'lose her rag' when I expected her to; she spontaneously picked up a book, which was unheard of before, and started reading; her turn taking improved and she was allowed to join a group for play who had previously ostracised her."
Anna's Mother; Anna is 8 years old; twelve neurofeedback sessions intensive.
"Julian's previous therapist suggested we go for an ASD assessment, having noticed some autistic traits in addition to his diagnosed ADHD and slower social development, along with tics, motor control issues and habits. After five sessions of neurofeedback, he had calmed a lot and was in full control of his impulsive aggressions when he didn't get something he wanted. His focus and general maturity improved incredibly in the twenty sessions we did in all, as did all of his other symptoms, as well as sleep."
Julian's Mother; Julian is 10 years old; twenty neurofeedback sessions in three months.
"Tamy's social fears and repetitive routines stopped and she regained her delightful demeanor. She started playing with children in her age group."
Tamy's Mother; Tamy is 3 years old; ten neurofeedback sessions in two months.
"Victor's anxities were getting incapacitating with the beginning of the new school year. Within five sessions, he was no longer getting panic attacks. His tutors noticed a new focus, and he found a great circle of friends at boarding school. He greatly enjoys his weekly two hour movie session."
Victor's Mother; Victor is 16 years old; twenty neurofeedback sessions in four months.
Neurofeedback lets us train dysrythmic brain areas. Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, it is solely auditory or visual, and the sensors are for measurement only.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the film showing on the screen; the training process is passive in this sense and all that is required of the person is to be engaged by the movie of choice.
Sessions can last from fifteen minutes to over two hours when tolerated. We generally achieve substantial calming in session that make previously unthought of film durations now attainable.
There are many approaches to mitigating stressors in an autistic child’s life.
Neurofeedback focuses on the brain: There are functional connectivity issues which we can identify and train.
Every autistic person is different. A brain map reveals individual challenges, which we address with Personalised Brain Training.
Initial effects are usually noticeable calming, reduced fear and stress, and improved behaviour. We have achieved this in as little as five sessions.
Improved sensory integration and social functioning can take longer, and we have had impressive results with intensive training over a week, or 10-15 sessions (see Case Study below).
Speech and motor issues can take longer to resolve, often of the order of 30-50 sessions, or even considerably more, depending on severity and training rhythm.
Small changes can make a world of difference. Ideally, we can start training early enough so that the child is able to express its needs and emotions before reaching a level of physical maturity that introduces substantially higher, and more restrictive care requirements.
Time and funds spent on neurofeedback training can yield impressive returns:
– emotional satisfaction of enabling a person fulfil more of their potential, and reduced stress and fear
– substantially reduced care costs and efforts
– potential for a person to reach financial independence.
Neurofeedback training has been shown to be a safe, feasible, and effective therapy approach to Autism Spectrum Disorder across all ages.
Multiple studies confirm:
– improved cognitive flexibility
– improved facial recognition
– better behaviour, including being less aggressive, more cooperative and better at communication
– improved functional connectivity in the social brain regions.
A 9 point improvement in IQ was reported alongside decreased ASD symptoms including attention, anxiety, aprosodias, social functioning, as well as academic and intellectual functioning.
Sensorimotor behaviour (posturography) improved in children.
Neurofeedback training has proven calming effects.
Research evidence for comorbidities, e.g. ADHD, dyslexia, depression, anxiety, seizures, sleep and behaviour is shown under the relevant tabs below.