Neurofeedback for Neurodegenerative Conditions
Daniel Webster’s Neurofeedback has produced strong results with neurodegenerative conditions.
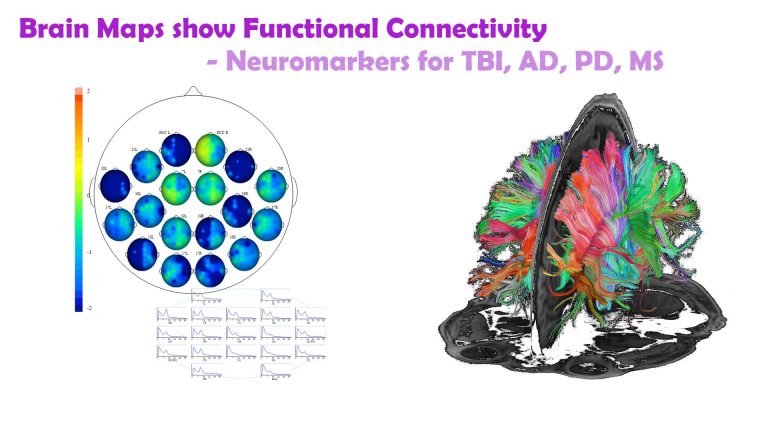
A qEEG brain map lets us identify neuromarkers in early stages, prompting sooner access to treatment.
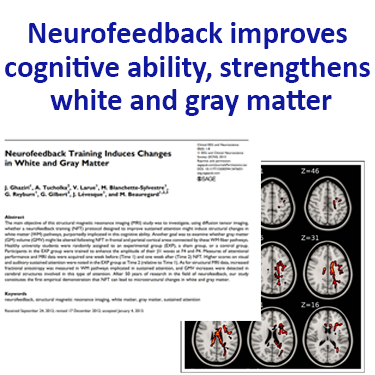
Neurofeedback has been shown to make positive structural improvements to the brain, improving myelination.
Symptom reduction, improved movement and sensory integration are evidence-based.
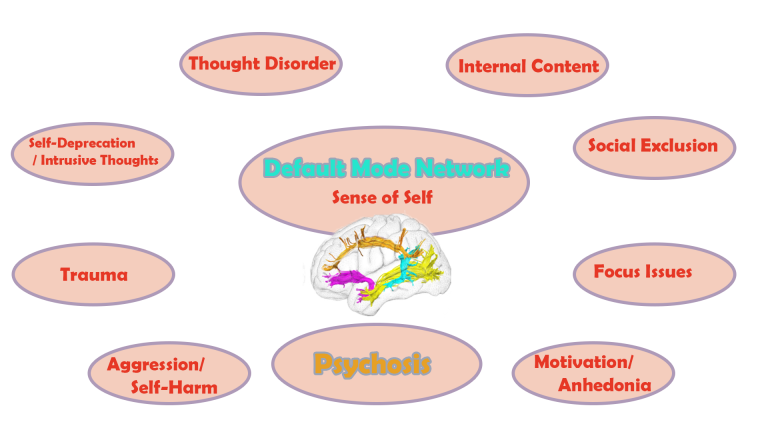
Secondary mental health issues, such as trauma, mood control, anxieties, sleep issues and impulsive aggression can also be addressed with neurofeedback training.
Early Detection

Neurodegenerative Conditions have neuromarkers which we can detect in pre-prodromal stages with a qEEG brain map.
Structural Improvements
Neurofeedback is shown to improve myelination, microglial function, cerebral blood flow, and hypo-/hypermetabolism, as well as functional connectivity
Quality of Life
Reducing symptom severity and addressing secondary mental health issues such as sleep, mood, sense of self, improves quality of life
Brain Maps can show us vulnerability to neurodegenerative conditions in an early stage.
Personalised Brain Training – qEEG brain map-based neurofeedback training – has been shown to provide the following with regard to neurodegenerative disease:
– reducing symptom severity
– structural improvements of the brain including myelination, microglial function, cerebral blood flow, hypo-/hypermetabolism
– ameliorating motor symptoms and sensory integration
– restoring life quality
– improving sleep, depression, anxiety and sense of self, as well as other concomitant mental health issues
Neurodegenerative Conditions include Parkinson’s, Alzheimer’s and Huntington’s Disease; MND / ALS; Dementia with Lewy Bodies (DLB) and Multiple Sclerosis. Many of these can lead to dementia.
Neurofeedback training is an evidence-based, non-specific, complementary therapy. It is drug-free and non-invasive.
Alzheimer's

There are neuromarkers for Alzheimer’s Disease in early stages of its progression.
We can detect this in pre-prodromal stages with a qEEG brain map.
Parkinson's
Research shows that neurofeedback can improve motor symptoms, balance, sensory integration and quality of life in PD.
Multiple Sclerosis
Neurofeedback can strengthen myelenation of white matter tracts and lead to cognitive improvement in MS and Huntington’s.
Brain Maps for Early Discovery
Brain maps show functional connectivity, and when this becomes impaired we detect vulnerability to a variety of conditions.
Some neurodegenerative conditions have non-specific neuromarkers which we can detect in the early stages of development. This can help seek diagnosis and life-enhancing treatment options.
qEEG brain maps are non-invasive and can be done at the client’s home.
They also reveal vulnerability to many secondary mental health conditions.
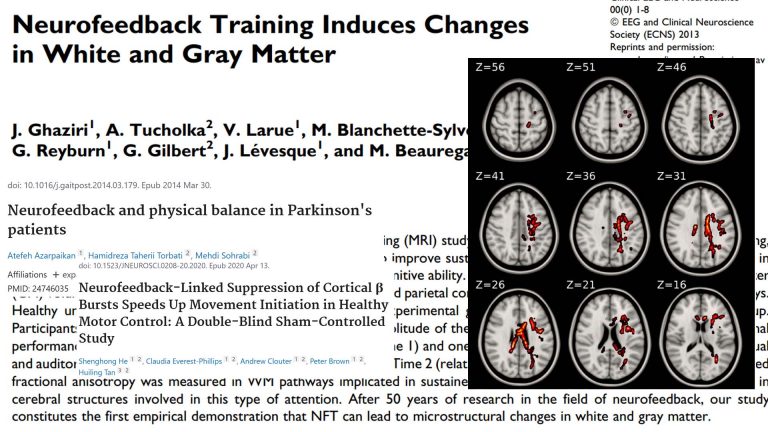
Neurofeedback Strengthens White Matter Tracts
White matter tracts are information superhighways connecting various brain regions and make up c.50% of our brain volume. White matter abnormalities in various forms of dementia, including DLB, Alzheimer’s and Parkinson’s, and mTBI (mild traumatic brain injury) are well documented, and these contribute towards cognitive decline.
With neurofeedback, we can train white matter tracts. This seminal study indicates that we can improve myelination with neurofeedback training. It has been further corroborated since, notably with regard to efficiency.
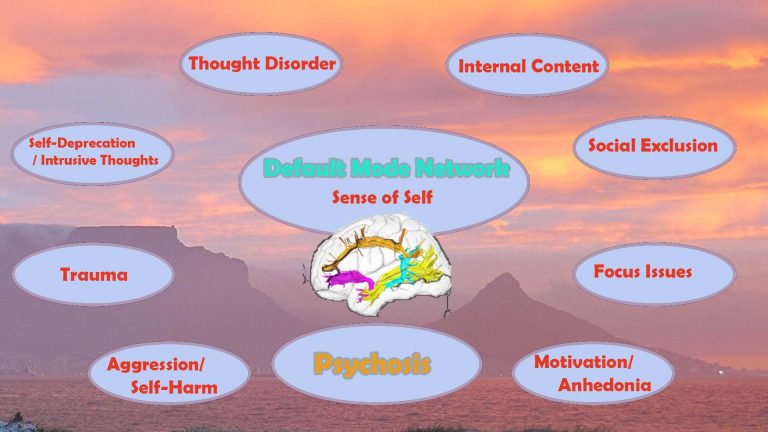
Neurofeedback for Secondary Symptoms
Neurodegeneration affects functional connectivity between brain areas and impairs the integrity of key networks.
Sufferers of neurodegenerative conditions experience mental health issues including depression, anxiety, loss of sense of self, sleep issues, and show general symptoms of trauma.
Behavioural issues arise, including impulsive aggression, rage, lack of focus and motivation.
Neurofeedback training is an evidence-based way of addressing each of these in a non-invasive, medication-free way.
Maintaining quality of life is an important part of any therapy.
Neurofeedback and Alzheimer's Disease (AD)
Alzheimer Disease (AD) is the most common neurodegenerative disorder. Similar to Parkinson’s Disease, secondary symptoms are neuropsychiatric in nature and can be addressed with neurofeedback training, helping the person to maintain their sense of self, mood regulation and sleep, and contain arising anxieties.
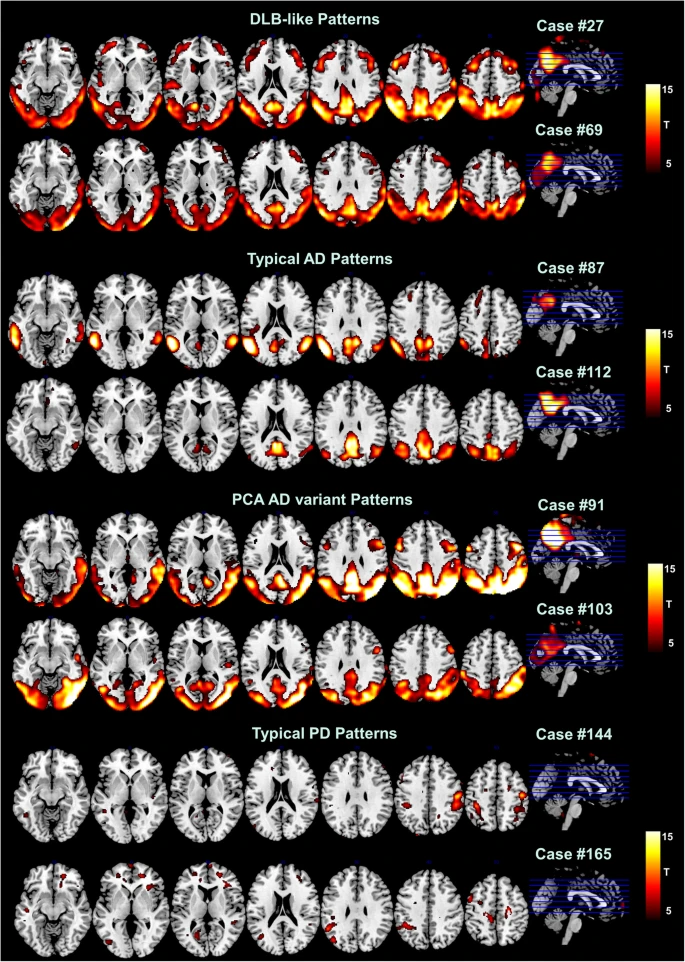
There are biomarkers that allow us to differentiate between Dementia with Lewy Bodies (DLB), Parkinson’s Disease, and Alzheimer Disease. A Kaiser Neuromap gives us a non-specific indication of each, that can assist early onset diagnosis and thus shape the treatment plan at an early stage.
Neuroplasticity is the process by which neurons form new synapses, or connections, and this ability is highly adaptive during both health and disease. Neurofeedback has been shown to promote this process.
Intra-day fluctuations in performance and function in persons affected by a neurodegenerative condition imply that neuronal loss (or gain) is not the only mechanism at work. The connectivity of neurons – their ability to form networks which contribute to memory and thought formation and ultimately our sense of self – is variable.
We also believe that maintining client functionality in the optimum range can help shape more positive trajectories.
As with other neurodegenerative disorders, physical changes in the brain affect our sensory interpretation of our surroundings, giving rise to neuropsychiatric disorders. We can become relational in our thinking, and specifically with regard to brain areas that are responsible for our interpretation of personal space and social boundaries.
Neurofeedback Personalised Brain Training aims precisely at encouraging cortical participation and help us share a reality with others, counteracting progression of major secondary, and possibly primary symptoms. Rather than promoting a ‘cure’, we are helping affected persons improve their quality of life in many ways.
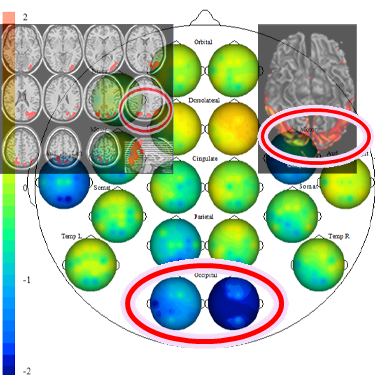
With a Kaiser Neuromap, we can see vulnerabilities to comorbid mental health conditions as well as:
— neuromarkers for early detection, e.g. Alzheimer’s, Dementia with Lewy Bodies (DLB), Parkinson’s Disease
— while not a diagnostic tool, qEEG- based Kaiser Neuromaps can show an early indication of possible dementia onset
— this can be confirmed via fMRI or other testing that is usually only performed in more advanced stages
— helps patient plan, make lifestyle changes, gain interoceptive awareness of own perception vs that of others
— enables patient to remain functional for longer
— reduces perception mismatches between client and environment
— improves manageability of disease progress.
Link between Alzheimer's Disease and Herpes Simplex Virus 1
The link between Alzheimer’s Disease and Herpes simplex virus type 1 (HSV1) has long been established, as summarised in this research paper from 2014. Four out of five people carry the herpes virus, with one in four being prone to physical symptoms upon periodic reactivation, e.g. blisters / cold sores occurring during times of stress and/or immunosuppression. Reactivated HSV1 has been found to cause inflammatory damage directly, probably involving increased formation of beta amyloid and AD-like P-tau changes found in HSV1-infected cell cultures. HSV1 DNA was found to be specifically localised in amyloid plaques in AD. Further links have been discovered between shared pathways of HSV1 and AD. HSV1 (herpes virus) can cross the blood-brain barrier and remain latent in the brain; combined with carriage of a type 4 allele of the apolipoprotein E gene (APOE-e4), this confers a high risk of developing Alzheimer’s Disease. Some 25-30% of the population carry this gene.
COVID-19 and Alzheimer's Disease
COVID-19 is of particular concern with respect to Alzheimer’s Disease. A pre-existing AD diagnosis is the single highest risk indicator of Covid infection identified thus far; the highest mortality is observed among the most elderly AD patients.
This susceptibility is partly explained by the up-regulation of ACE2R receptors in the limbic regions of AD-affected brains. It is even hypothesised that amyloid-beta is involved in fighting cerebral Covid infection, similar to an observed process with regard to alpha-synuclein in PD and Covid, a defence mechanism that might result in higher levels in the long run.
Reactivation of HSV-1 can aggravate Alzheimer’s Disease processes, such as amyloid beta and p-tau production. It has been shown that Covid can reactivate HSV-1, in particular the S1 spike protein.
Alzheimer’s Disease is viewed as a prion disease, a feature that again puts it into context with Covid-19, a coronavirus whose S1 spike protein has prion-like qualities.
What Causes Alzheimer's Disease?
Alzheimer’s Disease is the number one cause for dementia, with no known effective treatments. Finding the ‘root cause’ of this condition in order to produce a targeted cure is further complicated by the fact that the definition of what constitutes AD is somewhat circular. We define the phenomenon by its symptoms:
– Amyloid beta (Ab) plaques: Ab(40-42) oligomers are prominent in AD brains, both in soluble form, where they are more toxic, and in dense plaques, which are thought to serve as reservoirs. These oligomers can cause synaptic dysfunction, dendritic spine damage and neuronal death. Their inflammatory effect includes activation of microglia, astrogliosis, overproduction of cytokines, and dystrophy of neurites. This leads to brain atropy, often first observed in the temporal lobes. The epsilon4 allele of ApoE (e4APOE) is a genetic risk factor thought to affect Ab metabolism; 25-30% of the population have this gene. Ab oligomers can also induce the formation of Neurofibrillary Tangles (NFTs):
– P-Tau: Neurofibrillary tangles of hyperphosphorylated tau (p-tau) is another defining feature of AD. These formations occur after Ab accumulations, though they are seen in frontotemporal dementia without Ab plaques and may also be a parallel, symbiotic phenomenon accelerating disease progression. The Ab / p-tau theory however only accounts for a fraction of the structural dementia comorbidities, and treatment strategies targeting these two aspects have thus far been unsuccessful. This necessitates additional theories:
– Neuroinflammation: While unclear whether this is a consequence or cause of the condition, neuroinflammation is deemed to a major contributor towards the progression and severity of AD, possibly more so than Ab accumulation and NFTs. All three of the above aspects are addressed by another causative, or at least contributory theory:
– Viral Infection: Herpes Simplex Virus (HSV) reactivation is highly correlated with AD; causes damage to the same brain areas that are affected in AD (herpes simplex encephalitis (HSE), induced by HSV, damages the hippocampus, temporal and frontal lobes); is found (by DNA analysis) in substantially all amyloid plaques; is known to alter Ab metabolism, CA2+ homeostasis, synaptic dysfunction and apoptosis in HSV infected neuronal and glial cells. Note that this pertains to carriers of the e4APOE allele, while HSV in the brain of non-e4APOE carriers confers a much lesser risk. At least 80% of the population carries HSV, with only one fifth exhibiting symptoms (e.g. cold sores in times of stress or immunodeficiency); 25-30% of the population carry the e4APOE allele.
The last point is particularly relevant: There are multiple approaches to arresting HSV reactivation (e.g. anti-virals, such as acyclovir, and also components of seaweed(!)), which appears to be the most promising approach addressing suspected cause. It also provides a link with Covid, and an explanation for the high susceptibility of AD patients to this:
Covid, especially the S1 spike protein, has been shown to cross the blood brain barrier (BBB) and enter the brain through a number of pathways, including olfactory and vagus nerve. It has been found to reactivate latent cerebral HSV-1. Amyloid beta (Ab) (1-42) has been found to strengthen the binding of the S1 spike protein of Covid (SARS-CoV-2) to ACE2 receptors and increase viral entry. Covid also increases neuroinflammation. Further, the CA2+ dysregulation in AD facilitates passage of the Covid virus. ACE2 receptors are more prevalent in limbic regions of the brain, including brainstem and hippocampus, and importantly, they are up-regulated in AD brains, thus conferring higher susceptibility. Another possibility is that beta amyloid formation increases in response to HSV (and potentially Covid), as a defence mechanism, resulting in higher aggregation. An analogy is an observation made with influenza viruses, in particular the West Nile Virus, where alpha synuclein production increased to combat the virus (an absence thereof resulted in disastrous disease progression), leading to aggregation and thus higher Parkinson’s Disease susceptibility.
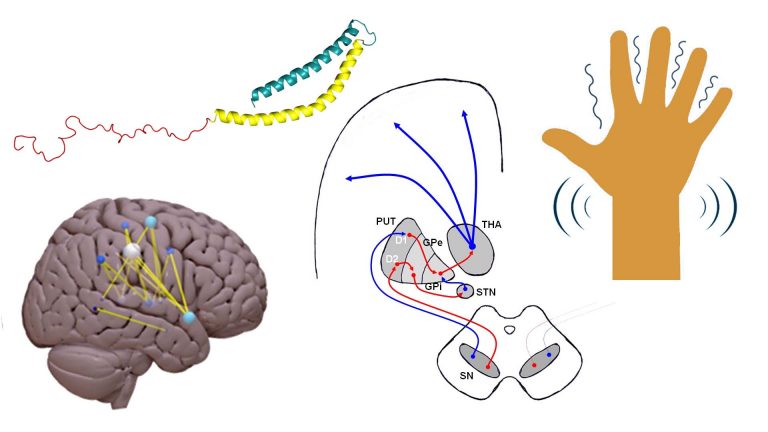
Neurofeedback and Parkinson's Disease (PD)
Parkinson’s Disease is the second most common neurodegenerative disorder, after Alzheimer disease (AD).
Onset is usually characterised by motor symptoms: bradykinesia (slowness of movement), rigidity, resting tremor and instability of posture.
REM sleep disorder in Parkinson’s sufferers has been shown to predict worse disease progression. In turn, REM sleep is a function of Default Mode Network deactivation.
With regard to PD, Neurofeedback training has been shown to improve:
– speed of movement initiation
– increased sensory integration in 10-12 sessions
– reduced symptom severity
Secondary, non-motor symptoms evolve, such as cognitive impairment, depression, sleep issues (e.g. REM sleep behaviour disorder (RBD), a potential prodromal marker of PD, where paradoxically motor function is improved relative to wake state), and olfactory dysfunction.
Neurofeedback is effective at reducing symptom severity and addressing most of these neuropsychiatric disturbances in healthy patients; while not shown to be a ‘cure’, quality of life improvement can be substantial.
On a cortical level, PD involves the loss of dopaminergic neurons, accumulation of Lewy bodies, damage to neuroglial cells and demyelination of neuronal axons.
Neurofeedback training has been shown to improve myelination across white matter tracts. We can also train frequencies that pertain to glial cells, potentially improving their self-regulation.
A recent study raised the spectre of a connection between COVID-19 infection and Parkinson’s; three persons without familial history developed clinical parkinsonism within 2-5 weeks following infection requiring hospitalisation.
Neuroplasticity is the process by which neurons form new synapses, or connections, and this ability is highly adaptive during both health and disease. Neurofeedback has been shown to promote this process.
Intra-day fluctuations in performance and function in persons affected by a neurodegenerative condition imply that neuronal loss (or gain) is not the only mechanism at work. The connectivity of neurons – their ability to form networks which contribute to memory and thought formation and ultimately our sense of self – is variable.
We also believe that maintining client functionality in the optimum range can help shape more positive trajectories.
As with other neurodegenerative disorders, physical changes in the brain affect our sensory interpretation of our surroundings, giving rise to neuropsychiatric disorders. We can become relational in our thinking, and specifically with regard to brain areas that are responsible for our interpretation of personal space and social boundaries.
Neurofeedback Personalised Brain Training aims precisely at encouraging cortical participation and help us share a reality with others, counteracting progression of major secondary, and possibly primary symptoms. Rather than promoting a ‘cure’, we are helping affected persons improve their quality of life in many ways.
General (non-PD specific) effects of neurofeedback training include:
– overall increased fine motor skills
– boost behavioural performance and learning
Comorbid mental health issues, such as anxiety, depression, aggression, and mood imbalances can be addressed directly with neurofeedback.
Chronic Pain is another application for neurofeedback, where studies have demonstrated its efficacy.
Subjectively, PD sufferers find neurofeedback training calming, reassuring and report an improved sense of feeling being part of their body.
Neurofeedback reduces Hallucinations
Hallucinations are a frequent occurrence in dementia sufferers – 80% of DLB (Dementia with Lewy Bodies) patients experience visual hallucinations, and these are complex visual, animate and often involve people. They are also a feature in other forms of dementia.
Research on audio-visual hallucinations in Schizophrenia patients have found that Neurofeedback training can produce significant results in reducing treatment resistant auditory verbal hallucinations. In 30% of cases antipsychotic medication has little or no effect. Psychotropic medication use in general can have undesirable side effects and is contentious.
Hallucinations have cortical sources – there are specific brain areas responsible for visual mental imagery, and research shows that the phenomenon as experienced by dementia sufferers correlates with decreased gray matter volume in various prefrontal, motor and visual association areas. Interestingly, the brain areas affected are differ by form of dementia, such as DLB versus Parkinson’s.
This suggests that treatment could be improved without side effects.
Research funded by Parkinson’s UK regarding hallucinations is currently focused on CBD and anti-sickness pills, and possibly other drugs. Neurofeedback training is drug-free and non-invasive complementary therapy.
Neurofeedback and Multiple Sclerosis, Huntington's Disease
It has recently been shown that neurofeedback training led to cognitive improvements in Multiple Sclerosis (MS) patients, and that this corresponded to improved functional connectivity in key motor and salience networks. Increased fractional anisotropy (FA) was observed, which correlated with cognitive improvement.
MS is a neurodegenerative condition that adversely affects axonal myelination. FA is among other a measure of myelination, so the result that neurofeedback can make positive changes in this condition is very encouraging.
Lesions in MS present first in the corpus callosum, a fibre bundle linking left and right brain hemispheres. With a Kaiser Neuromap, we can detect changes in functional connectivity here, which can serve as an early indicator to prompt further investigation at an early stage, while being a complementary approach that is not a substitute for full examination. Neurologists have appreciated this input.
A study with sufferers of Huntington’s Disease, another neurodegenerative condition, showed that cognitive and motor skills improved and that these changes related to improved functional connectivity in key brain regions, again a conclusion that neuroplasticity can be induced despite the presence of neurodegeneration.
Neuroplasticity is the process by which neurons form new synapses, or connections, and this ability is highly adaptive during both health and disease. Neurofeedback has been shown to promote this process.
Intra-day fluctuations in performance and function in persons affected by a neurodegenerative condition imply that neuronal loss (or gain) is not the only mechanism at work. The connectivity of neurons – their ability to form networks which contribute to memory and thought formation and ultimately our sense of self – is variable.
We also believe that maintining client functionality in the optimum range can help shape more positive trajectories.
As with other neurodegenerative disorders, physical changes in the brain affect our sensory interpretation of our surroundings, giving rise to neuropsychiatric disorders. We can become relational in our thinking, and specifically with regard to brain areas that are responsible for our interpretation of personal space and social boundaries.
Neurofeedback Personalised Brain Training aims precisely at encouraging cortical participation and help us share a reality with others, counteracting progression of major secondary, and possibly primary symptoms. Rather than promoting a ‘cure’, we are helping affected persons improve their quality of life in many ways.
The ability of white matter disruption to contribute towards cognitive decline to the extent that dementia results is known since the 1980s when the term “White Matter Dementia” was coined. Various pathologies, including Parkinson’s, Alzheimer’s, Huntington’s, ALD and MS (Multiple Sclerosis) are significantly characterised by white matter disruption. In fact, the involvement of white matter disruption in these neurodegenerative pathologies has been asserted with a certainty that contrasts with the evolution of attempts to define the various ‘diseases’ at times.
Neurofeedback can positively affect white matter growth. In healthy patients, this growth was faster than the rate of neurodegeneration in neurodegenerative conditions. Research has yet to confirm that this works for these conditions specifically.
This approach is non-specific and holistic – we are treating the brain as a whole, and not with regard to a particular condition. Indeed, defining a neurodegenerative pathology is in itself a challenge – Parkinson’s diagnostic criteria have evolved substantially in recent decades and are still subject to debate and expansion, as is the definition of a disease itself. In vivo, that is, before a post mortem examination, Parkinson’s is largely ascertained on the basis of symptoms. It would seem logical to aim therapy at these symptoms, rather than, say, chase a ‘cure’ for an ill-defined phenomenon (is it strictly, and only, dopaminergic neuron death?). This differentiation in approach is important as funding criteria for research into ways to ameliorate the condition often utilise this to the detriment of alternatives. As a result, neurofeedback is sadly neglected in the quest for helping people with neurodegenerative conditions.
Neurofeedback has been shown to help with primary and secondary symptoms in Parkinson’s; it is a non-specific, complementary therapy that is non-invasive and medication-free.
White matter decline is measurable with DTI (Diffusion Tensor Imaging) even before the onset of cognitive decline. The mechanisms by which damage occurs varies by pathology. However any intervention that improves these connections should have a positive effect on the person, both structurally and cognitively. Counteracting this trend in a non-invasive, medication-free and enjoyable manner seems a worthy cause.
The search for a ‘cure’ of different neurodegenerative conditions which lead to dementia is strongly focused on the defining feature – e.g. amyloid beta production in Alzheimer’s, and dopaminergic neurons in Parkinson’s. Addressing symptoms is often seen as a secondary endeavour, with regard to time, prestige, funding and resources. Daniel Webster has spent time working in palliative care and high-support living and rehabilitation facilities. He found that ameliorating life quality can lead to at least a perceived slowdown in the progression of a condition. There is also a possibility that symptom reduction can actually impede a worsening of the condition, and certainly worthy of further research.
Subjective feedback by dementia clients is very encouraging. Research into this aspect of dementia, and how neurofeedback can be applied to slow, arrest and potentially reverse disease progression, is a worthwhile endeavour. Please contact Daniel directly to support initiatives in this regard.
“The idea of Neurofeedback is very interesting and the evidence [above] shows great potential. Larger studies would be needed to fully understand the potential and safety of this method for people with Parkinson’s before we could share it with our community.” –Researcher Katherine Fletcher (PhD) of Parkinson’s UK
Reverse enquiries, from persons affected by Parkinson’s to charities seeking to represent their cause, could accelerate the inclusion of neurofeedback into research programmes funded by them, and awareness raising of a complementary therapy that has already been shown to produce positive effects on primary and secondary (e.g. mental health) symptoms, thus benefiting more people, in a timely manner.
Currently, few, if any, research aggregators (e.g. charities) make any mention of neurofeedback as a complementary therapy approach while admitting openness to exploring it should persons affected by the various conditions approach them. Unfortunately, the lack of mention reduces the propensity and likelihood of such reverse enquiries. To break this cycle, the opportunity exists to directly fund, or engage in, neurofeedback training for sufferers of neurodegeneration and/or dementia.
The “larger studies” needed per Parkinson’s UK (above quote) also appear to face volunteer shortages, and at the time of writing (24 July 2022), five studies face the risk of being shut down as a result, with potentially millions of pounds of research funding (and donations) going to waste. The hope of “larger studies” being conducted with regard to neurofeedback thus seems a very distant prospect.
The point of this discourse is to illustrate the dynamics at play when it comes to awareness raising for neurofeedback for sufferers of neurodegeneration and its secondary (mental health) effects. There are already studies (above) demonstrating efficacy, including with regard to primary symptoms. Daniel Webster has personally witnessed its beneficial effects with his late grandfather, 99, in a palliative care setting.
Daniel Webster is offering neurofeedback training to persons suffering from Parkinson’s, and other forms of dementia or neurodegeneration, on a sponsored basis and welcomes support from donors and persons looking to benefit from it.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
Neurofeedback and Parkinson's Disease (PD)
Parkinson’s Disease is the second most common neurodegenerative disorder, after Alzheimer disease (AD).
Onset is usually characterised by motor symptoms: bradykinesia (slowness of movement), rigidity, resting tremor and instability of posture.
With regard to PD, Neurofeedback training has been shown to:
– improve static and dynamic balance
Secondary, non-motor symptoms evolve, such as cognitive impairment, depression, sleep issues (e.g. REM sleep behaviour disorder (RBD), a potential prodromal marker of PD, where paradoxically motor function is improved relative to wake state), and olfactory dysfunction.
Neurofeedback training is effective at reducing symptom severity and addressing most of these neuropsychiatric disturbances.
On a cortical level, PD involves the loss of dopaminergic neurons, accumulation of Lewy bodies, damage to neuroglial cells and demyelination of neuronal axons.
Neurofeedback training has been shown to improve myelination across white matter tracts. We can also train frequencies that pertain to glial cells, potentially improving their self-regulation.
A recent study raised the spectre of a connection between COVID-19 infection and Parkinson’s; three persons without familial history developed clinical parkinsonism within 2-5 weeks following infection requiring hospitalisation.