Neurofeedback for ADHD
Fast, Transformational Results.
ADHD is characterised by a persistent pattern of inattention, and/or hyperactivity and impulsivity that interferes with functioning and development.
With Daniel Webster’s qEEG Brain Map, we can attribute character traits, such as ADHD symptoms, to dysrhythmia of particular brain areas. While not providing diagnosis, we are able to disaggregate the heterogeneous manifestations of this, and other, conditions, and provide a personalised assessment of vulnerabilities that extend beyond focus and inhibition control issues.
Impaired social interactions, lack of productivity, and excessive energy exertion for little gain result in lower expectations regarding developmental trajectories.
With Daniel Webster’s Neurofeedback, we can help the brain become more flexible, mature and integrated. This enables better focus, productivity and social integration and resets trajectories, thus improving quality of life and promoting the full realisation of talents and potential.
The process is non-invasive, evidence-based, and enjoyable.
Daniel practices in London and Edinburgh, and is available for home visits internationally.

Client Feedback
Overview of Daniel Webster's Neurofeedback for ADHD

Changing Trajectories
Developmental expectations and trajectories are dampened by reduced productivity and focus, social integration and cognitive inflexibility, and resultant higher support or support care requirements.
Early intervention can reduce this gap with peers and produce virtuous feedback loops.
Daniel Webster’s Neurofeedback produces transformational results in all age groups, from young children to adults.
Personalised Training
qEEG brain maps are a non-invasive way of analysing functional connectivity of over 40 brain areas, a measure of the health of the brain’s ‘wiring’, or relative contribution of each component.
There are common neuromarkers in persons with an ADHD diagnosis (note we do not provide diagnosis). ADHD is a heterogeneous condition, often with other comorbidities, requiring a personalised approach, bespoke to the person’s challenges.
Daniel Webster’s Neurofeedback is personalised brain training that is enjoyable – the person watches a movie of choice, the feedback is subtle (not stop-start) and training is passive, requiring only attention to the movie.
See here for more information on How it Works.

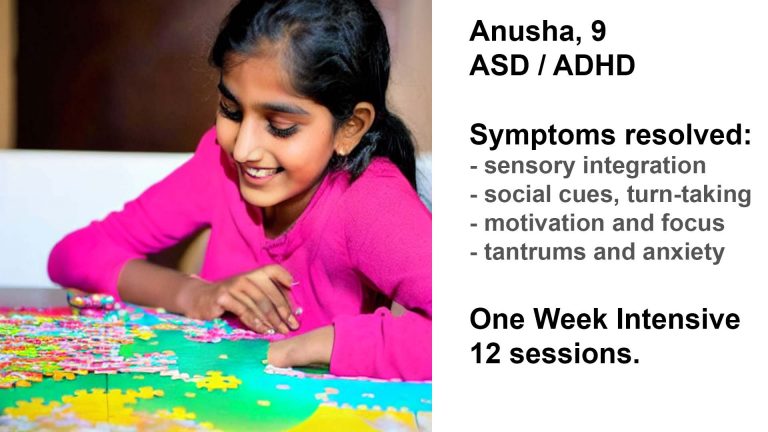
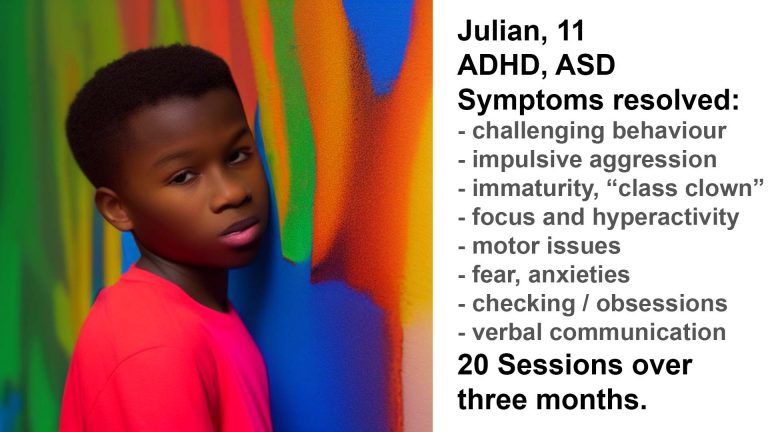
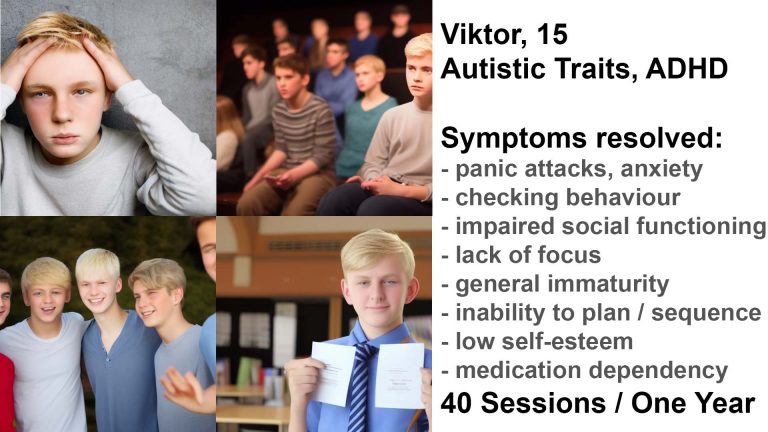
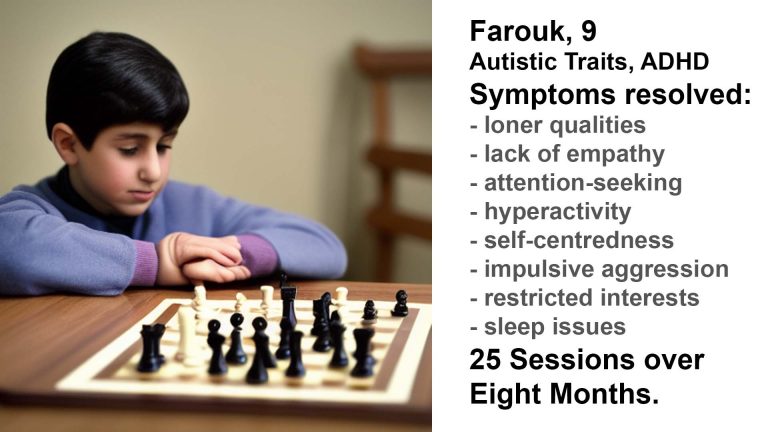
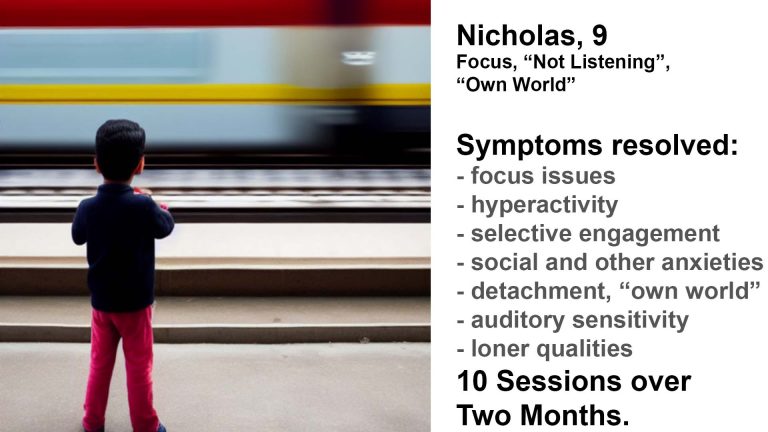
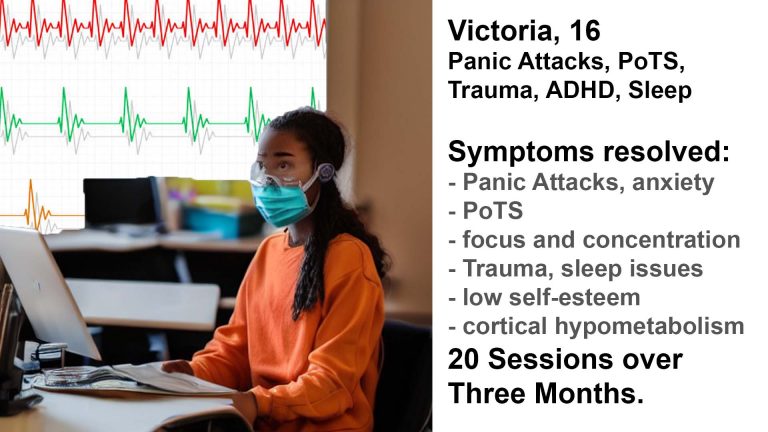
Case Studies
Daniel’s Neurofeedback is personalised and suited to all age groups.
Early interventions can resolve developmental gaps with peers and accelerate maturation.
Adult ADHD usually presents with other comorbidities, such as anxieties, social interaction challenges, sleep issues, mood control and impaired sense of self. Personalised Brain Training can address these.
Fast, transformative results from age 2 to adults are summarised in the case studies below.
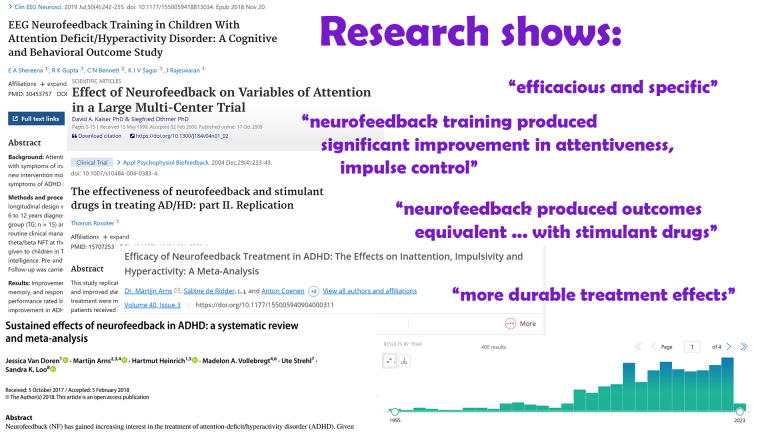
Research
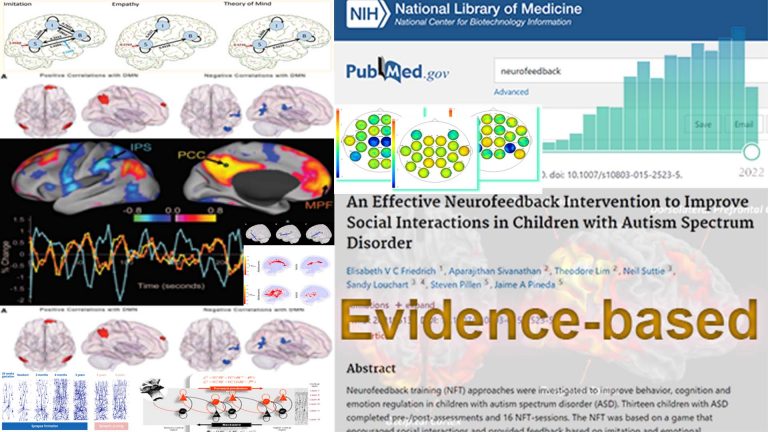
Neurofeedback is evidence-based, with over 2,800 supporting studies.
Over 370 research reports shows that Neurofeedback for ADHD generates lasting improvement in executive function, attentiveness and impulse control, “equivalent to those obtained with stimulant drugs”. It is “efficaceous and specific” with “no significant contraindications”.
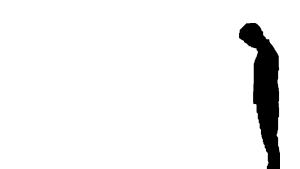
The pro-social effects are produced by beneficial changes in functional connectivity.
Neurofeedback is non-invasive, evidence-based and medication-free.
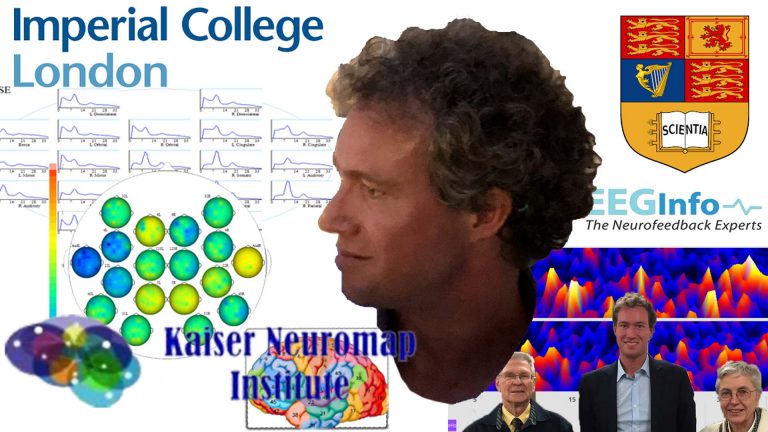
Daniel Webster
Daniel Webster uses the most advanced neurofeedback methods.
He was taught in LA by the founders of the field, Dr. David Kaiser and Sue & Siegfried Othmer.
Daniel continues to research and advance neurofeedback protocols, and has recently presented at Africa’s first conference for autism and neurodevelopmental disorders.
Case Studies
Daniel Webster uses the most sophisticated and insightful qEEG interpretation methodology to reveal individual issues and form a neurofeedback training plan.
Aspects of ADHD

Personalised Approach
ADHD is a heterogeneous conditions, and a brain map lets us understand the specific challenges a person is facing. With neurofeedback, we are helping in numerous ways:
– reduce fear, auditory sensitivity and anxieties
– strengthen key brain network functionality to improve predictive capacities and abstraction abilities / learning
– reduce inclination towards impulsive aggression, and further rage, when outcomes don’t match expectations
– restore/create ability to self-soothe and self-nurture
– improve planning, focus and motivation
– train self-other distinction capacity, appreciation of social boundaries, perception of other and social emotions.
Improved flexibility leads to an accelerated maturation and self-realisation.

Comorbidities
Two-thirds of children diagnosed with ADHD have one or more other mental health or neurodevelopmental conditions, beyond distractibility and/or hyperactivity. 46% show a learning disability, 26% conduct disorder, 18% anxiety, 14% depression, and 12% speech problems.
With a brain map, we can assess dysrhythmia of brain areas that contribute towards various aspects of functionality, and then address these with neurofeedback training in a personalised manner.
Rather than addressing a specific pathology – brain maps do not provide diagnosis – we help improve overall brain function. Furthermore, we have a chance at promoting structural improvements, such as prefrontal brain maturity.

Motivation
Motivation: having sufficient drive, optimism, persistence and endurance to implement plans and overcome setbacks.
We often avoid things to do until the last moment, or are simply not motivated to take on tasks, especially complex ones with less immediate gratification. Once we are engaged, we can dedicate our attention intensely to an activity, often something repetitive.
There are brain areas governing our dopamine pathways, as well as monitoring and evaluating cost of effort vs. reward. We can train these with neurofeedback.
Self-esteem, an understanding of one’s own strengths and weaknesses, and the ability to self-soothe, that is, to rationalise thoughts, are also affected behavioural components.

Mood Control
There are numerous contributors to depressive tendencies from a neural perspective. A brain map lets us identify possible cortical contributors, and we can train important neural hubs that affect our ability to regulate mood.
In this sense, neurofeedback is a next-generation treatment for depression. We seek to avoid reliance on medication, especially from an early age.
The effectiveness of neurofeedback training in treating depression is well-documented. Effects have been shown to be strong and lasting. Working on depression helps us re-establish our sense of safety in the world, and often correlates with our ability to fall asleep.

Distractibility
A core issue of ADHD, Distractibility, can be disaggregated, as it is a function of various brain areas:
– Planning and Organisation: understanding goals, working back to the present and structuring a workflow conducive to achievement, seeing the bigger picture and dividing projects into tasks, prioritising these and being flexible.
The ability to form an overview of the task at hand, break this down into smaller, manageable steps, and sequence these accordingly, can be trained.
– Concentration: the ability not to be distracted and maintain attention on the relevant task at hand. Distractibility is a function of spatial awareness, and there are brain areas dedicated to this task. When they are dysrythmic, we become easily distracted.

Behaviour Issues
Behaviour issues include impulsive aggression when things don’t work out as expected, extending to protracted rage and obstinacy. Anger management and self-control are governed by brain areas which we can train.
We have seen impulse and mood control improve substantially within a few sessions.
“I wanted to mention that we have noticed improvement with Julian.
He is calmer, less reactive and when he gets frustrated he manages to calm himself down.
Not sure if it’s a temporary thing, but this weekend was all right :)”

Social Rules
Self-other differentiation, the ability to empathise and anticipate, synchronising with others, respecting social and personal boundaries are key developmental milestones which are governed by specific brain areas. Training these generally results in the person effectively recruiting others for their purposes – forming friendships.
We have seen impressive transformations within ten sessions of neurofeedback. Another quality we can assess for is relational thinking, where the person feels as though all sensory stimulus is directed at them and hence unable to take on different perspectives. Flexibility is the key virtue we strive for.

Coordination, Tics, Stutter
Our brain controls our movements. Functional connectivity dysregulation in ADHD can affect many of the brain areas involved in planning and executing motor actions. With neurofeedback, we can train these areas to improve symptoms in an evidence-based manner.
There are various cortical, and sub-cortical brain areas involved in motor coordination.
In our experience, the following issues can resolve with neurofeedback training:
– motor issues, such as dyspraxia and lack of coordination
– stutter and speech production
– facial tics
– uncontrolled, compulsive movements and actions.
Before and after brain maps corroborate these findings; research has so far focused on neuromarkers for these phenomena, and suggest neurotherapy as an adjunct to traditional therapies.
Tourette’s Syndrome can involve many of the above issues, as well as lack of executive control, again an aspect we have seen improve substantially with neurofeedback training.
Sensory Integration
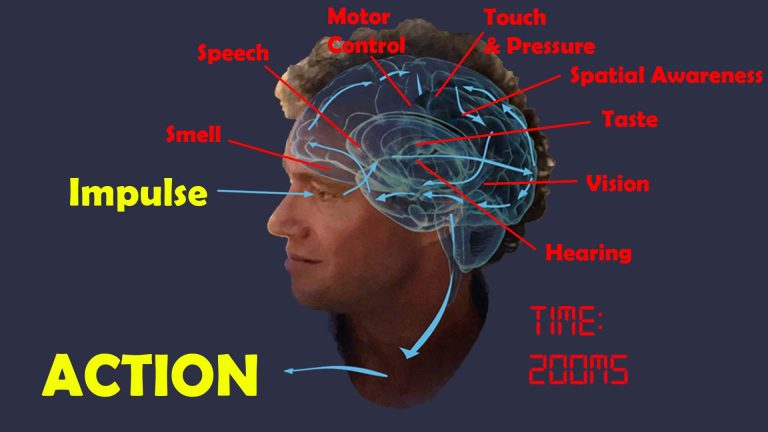
There are distinct brain areas that interpret the respective sensory input, and through various convergent processing stages – multi-modal association areas – the brain constructs a scene, and understands where we are with respect to our environment. For example, the back, or occipital area of our brain is where visual information is analysed; auditory processing occurs in the temporal lobe, close to our ears.
When any of these brain areas becomes dysrhythmic, our interpretation becomes distorted, for example, we can become hyper- or hyposensitive, as is seen in various symptoms of autism.
Individual sensitivities vary substantially. With a brain map, we can determine which particular sensory processing areas are vulnerable, providing a personalised approach.
With neurofeedback, we can train the brain areas relevant for efficient sensory processing and integration. Hypersensitivity to sound, as well as overly emotional interpretation of what is said, becomes attenuated and flexible. Body awareness and motor control improves, as does facial recognition. This is evidence-based, and confirmed by outcomes from our training.
Dyslexia, Dyscalculia
Dyslexia often presents together with ADD/ADHD and other behavioural issues. With a Kaiser Neuromap, we can assess vulnerabilities, and then train these with Personalised Brain Training.
Dyslexia is an impaired ability to understand written and printed words or phrases and affects 10-20% of the population in both males and females. The disorder can result in learning difficulties, poor academic performance, stigmatisation and ensuing behavioural issues.
While often classed as a disability, there are associated strengths: creativity, the ability to solve complex problems, unorthodox approaches to ideas and projects, and a more detached ability to apply logical thinking are some of these. Nonetheless, the condition can impair school and social functioning, slow maturation and significantly affect self-confidence and -esteem.
“Picked up a book and started reading! Unheard of before, I could never get her interested in reading for herself.” – Mother of Anna (9)
There are neural correlates with dyslexia which we can train with neurofeedback.
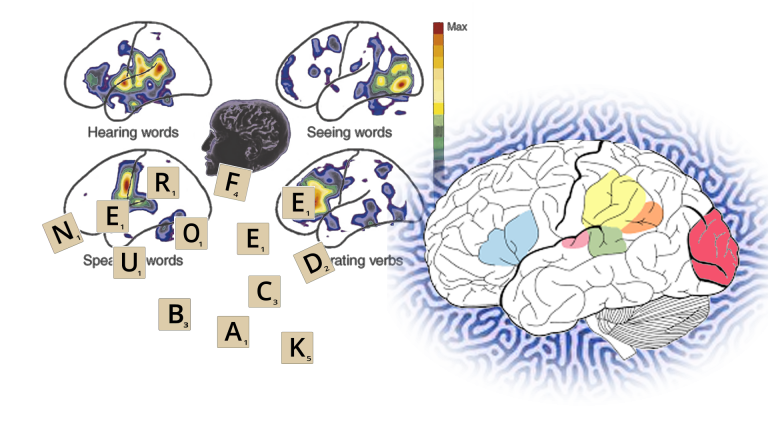
Reading and comprehension involves multiple brain areas as well as their seamless communication. We have Wernicke’s area for comprehension, and Broca’s for speech generation. Additionally, there are regions involved in sequencing, visual recognition, focus and attention, and contextualisation or syntax recognition of subject matter along with various memory-related areas.
It is important to note that there are different types of dyslexia. A brain map shows us which brain areas are dysrhythmic.
With neurofeedback, we train brain areas involved in visual and auditory processing; memory; focus and attention; syntax and context; sequencing and organisation. We also train the connections between these areas. The approach is holistic: we work on core networks, and their integration with each other.

Research: Dyslexia and Neurofeedback
Research has shown that neurofeedback training can improve reading ability and phonolocigal awareness deficit in children with reading disabilities, as well as improvements in spelling.
For a summary of 18 neuroscientific research studies on language learning impairment produced until 2015, see here.
Neurofeedback training was shown to improve speech-in-noise perception and auditory discrimination that was applicable post training and long-lasting. This shows that we can positively affect neural encoding of acoustic inputs in the auditory cortex, a frequent issue with autistic individuals.
In ADHD children, neurofeedback training improved visual memory, enhanced auditory short-term memory and auditory working memory.
Biofeedback produced better and more lasting effects than traditional therapy in behavioural dysphonia.
Neurofeedback was shown to improve the ability to identify emotional prosodic intonations.
Phonetic recognition and reading skills have been shown to improve with neurofeedback training, another important component of speech and language acquisition (see “Dyslexia”).
Personalised Brain Training is a holistic approach; we also train brain areas relating to focus, motivation and sense of self, as well as sequencing and motor skills, all of which contribute to the development of speech.
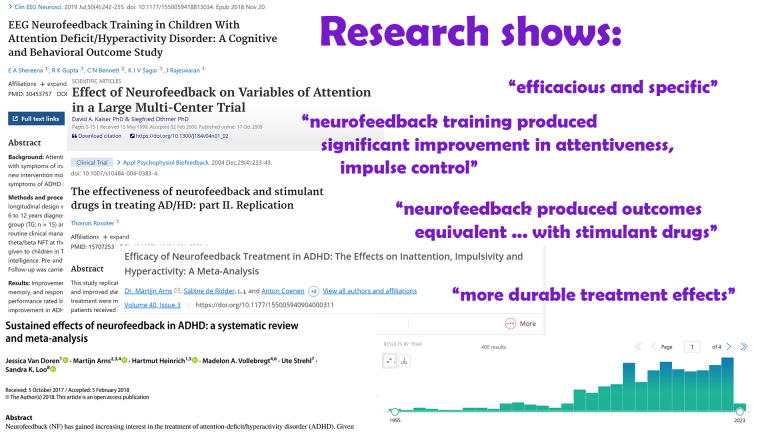
Research: Neurofeedback for ADHD
Research on Neurofeedback training for ADHD shows it is evidence-based and produces lasting results:
Attention deficit: Efficacy is well-documented – there are over 370 research reports on Neurofeedback and ADHD on PubMed.
In line with AAPB and ISNR guidelines for rating clinical efficacy, neurofeedback can be considered “Efficacious and Specific”, the highest level (5), with a large effect size for inattention and impulsivity in this study.
A large-scale study showed that neurofeedback is effective in remediating attentional dysfunction. Significant clinical improvement in one or more of attentiveness, impulse control, and response variability was observed in 85% of participants after 20-40 training sessions.
Impulse control and attention improved through neurofeedback training, producing “patient outcomes equivalent to those obtained with stimulant drugs”
Neurofeedback “appears to have more durable treatment effects, for at least 6 months following treatment.”
Neurofeedback was shown to be an effective method to enhance cognitive deficits, reduce ADHD symptoms and behaviour problems in children. The effect was maintained in a follow-up six months later.
There are numerous academic studies confirming the efficacy of EEG biofeedback (another name for neurofeedback) with sustained performance gains.
The American Academy of Pediatrics bases its conclusion that there are “no significant contraindications” to its use on these studies.
ILF / Othmer Method neurofeedback training was shown to reduce ADHD symptoms, specifically distractibility and impulsiveness, in a study involving 251 children over a course of 30 neurofeedback sessions.
Training specific brain areassuccessfully activated error monitoring networks in ADHD patients, associated with symptom improvements. Dynamic functional connectivity was found to be maintained in a follow-up 11 months later.
Another study attested improved response control and attention in ADHD post Neurofeedback.
Mood regulation and Motivation: see here
Working Memory: see here
Sense of Self: With Personalised Brain Training, we work on the Default Mode Network, the neural basis of self.

Approaches to ADHD
It is important to note that ADHD diagnosis (which we don’t provide) is based on behavioural observations / assessments rather than medical measurements, such as actual dopamine levels in the case of the dopamine deficiency hypothesis.
Daniel’s Neurofeedback relates behaviour patterns and character traits to the function, or maturity, of specific brain areas and networks – an evidence-based approach. With a brain map, we can assess vulnerabilites and then train them with neurofeedback, a non-invasive, enjoyable process involving watching movies.
Daniel’s Neurofeedback provides a more granular, and thus personalised approach to addressing a person’s presentation of challenges.
It is non-invasive, medication-free and evidence-based.
Emergence and Prospects
It is important to note that ADHD diagnosis (which we don’t provide) is based on behavioural observations / assessments rather than medical measurements, such as actual dopamine levels in the case of the dopamine deficiency hypothesis.
Daniel’s Neurofeedback relates behaviour patterns and character traits to the function, or maturity, of specific brain areas and networks – an evidence-based approach. With a brain map, we can assess vulnerabilites and then train them with neurofeedback, a non-invasive, enjoyable process involving watching movies.
Daniel’s Neurofeedback provides a more granular, and thus personalised approach to addressing a person’s presentation of challenges.
Dopamine Deficiency?
It is important to note that ADHD diagnosis (which we don’t provide) is based on behavioural observations / assessments rather than medical measurements, such as actual dopamine levels in the case of the dopamine deficiency hypothesis.
Daniel’s Neurofeedback relates behaviour patterns and character traits to the function, or maturity, of specific brain areas and networks – an evidence-based approach. With a brain map, we can assess vulnerabilites and then train them with neurofeedback, a non-invasive, enjoyable process involving watching movies.
Daniel’s Neurofeedback provides a more granular, and thus personalised approach to addressing a person’s presentation of challenges.
Medication
It is important to note that ADHD diagnosis (which we don’t provide) is based on behavioural observations / assessments rather than medical measurements, such as actual dopamine levels in the case of the dopamine deficiency hypothesis.
Daniel’s Neurofeedback relates behaviour patterns and character traits to the function, or maturity, of specific brain areas and networks – an evidence-based approach. With a brain map, we can assess vulnerabilites and then train them with neurofeedback, a non-invasive, enjoyable process involving watching movies.
Daniel’s Neurofeedback provides a more granular, and thus personalised approach to addressing a person’s presentation of challenges.
Julian's Story
Julian, just turned 11, introduced himself with “I’m Julian. I have ADHD”. His self-esteem was on the floor.
Shy and well-behaved, his demeanour contrasted with the behaviour issues his mother deemed most pressing. Her altercations with Julian were daily, prompted by incidences where things didn’t go as imagined or hoped for by him, and turning into a self-fuelling rage that would spoil the entire weekend. His focus was poor, conversations marred by distractions (“jibberish”, in her words), relative maturity low for his age group and he fortunately attended a school that catered for his academic performance and social needs.
A year of psychotherapy almost landed him with an autism assessment, and he hated the various other therapeutic procedures he had to endure that aimed at helping his physical coordination issues.
Within two weeks, or four sessions, his behaviour had taken a turn; in his mother’s words:
"I wanted to mention that we have noticed improvement with Julian.
He is calmer, less reactive and when he gets frustrated he manages to calm himself down.
Not sure if it's a temporary thing, but this weekend was all right :)"
Continued Training from Sessions 5-20
Far from temporary, his maturation accelerated noticeably in the following weeks.
A family trip was described as “the best vacation we’ve ever had!” by his mother. While on holiday, he learned to scuba dive, and his parents noticed that he was asking coherent, thoughtful and relevant questions during the instruction. Anxieties and fears dropped noticeably, attention and focus improved, childish behaviour – such as “class clown” attempts at drawing attention – ceased, and he became involved in extracurricular school activities.
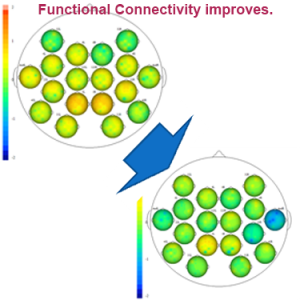
Julian’s brain maps confirmed the transition he was going through. He had skipped years of physical maturation that should have taken place, especially in his prefrontal cortex. Functional connectivity of brain areas responsible for behaviour, focus and sense of self had improved substantially, as – notably – had his motor skills. Julian’s trajectory has changed from spiralling into lower depths of special needs diagnoses, to establishing a confident, engaged and healthy risk-taking personality. With these new acquired powers, he is able to shape his own future in a way that helps sustain his progress.

Does it last? Yes. A year later Julian is thriving at school and socially.
We all evolve, and life throws us challenges. Key to improvement is being equipped with the right tools – cortical maturity and functional connectivity in this case – that help us create positive feedback loops within our environment.
Twenty sessions helped liberate this young man immensely. With neurofeedback training we can address developmental issues.
Brain Maps and Personalised Brain Training Explained
Personalised Brain Training with Neurofeedback
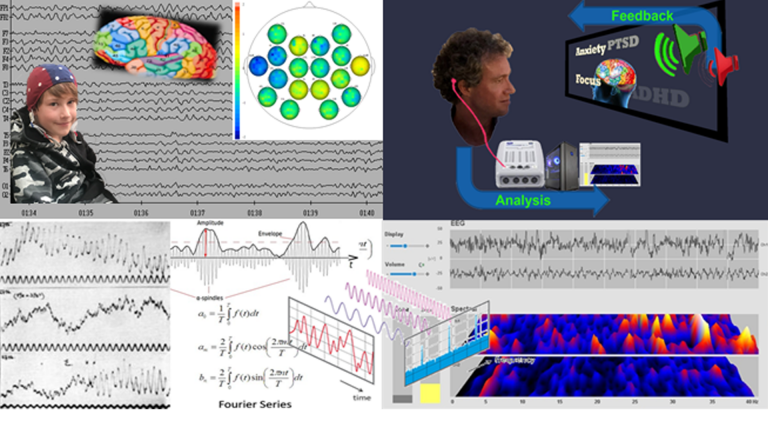
Neurofeedback lets us train dysrythmic brain areas. With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, short and instantaneously.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the movie; the training process is passive in this sense.
The drop in volume is subtle, so we continue to understand the flow of the movie. No current or electrical stimulation is fed to the brain; sensors simply read brainwaves and the feedback is purely audio-visual.
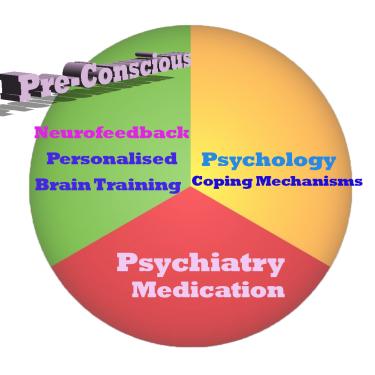
Neurofeedback trains our Pre-Conscious Mind
Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
This equips us with the ability to live in the moment and attain our potential (if we have to resort to conscious control, we are not living in the moment).
We take a holistic approach to healthy brain self-regulation, rather than categorisation or diagnosis.
Personalised Brain Training is an advanced qEEG brain map-based approach to neurofeedback training developed by the founders of the field. Taking Othmer Method / ILF training methods further, it employs Default Network Training protocols as developed by David Kaiser.
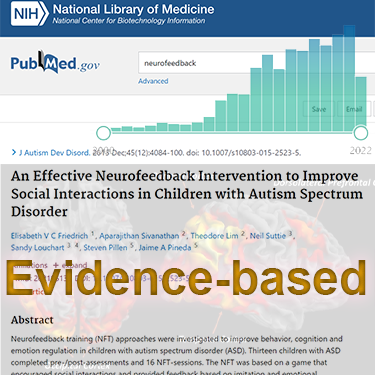
Neurofeedback is Evidence-based
Neurofeedback training is an evidence-based complementary therapy. Its efficacy was first demonstrated some 50 years ago, and with advances in technology, training protocols have become more efficient and the feedback method – watching movies – thoroughly enjoyable.
Neurofeedback is evidence-based. It’s first application was discovered in 1971 when it was used to resolve intractable epilepsy.
There are over 2,000 peer-reviewed research reports on PubMed demonstrating efficacy across a number of pathologies.
In the US, it is an accepted complementary treatment for many challenges.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
The Process Explained
Step 1: Brain Map
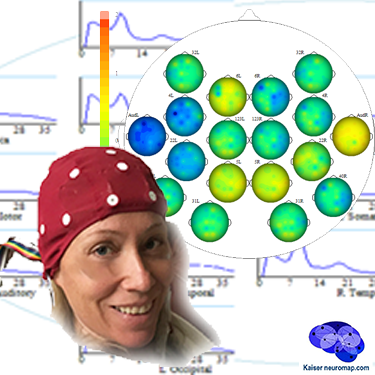
A qEEG recording takes about 45minutes for a 20 minute recording.
A cap with 19 sensors is is fitted to our head and gels inserted to ensure connectivity. The sensors only read – there is a tiny voltage on the surface of our head that these pick up. The gels are easily washed out later. This is also the last time we wear the cap (until a remap after ten sessions); training is done with single sensors.
We analyse the data with Kaiser Neuromap software which gives us a unique view into character traits and vulnerabilities.
Findings are presented in a separate one-hour conversation where we discuss the key elements.
Step 2: Neurofeedback
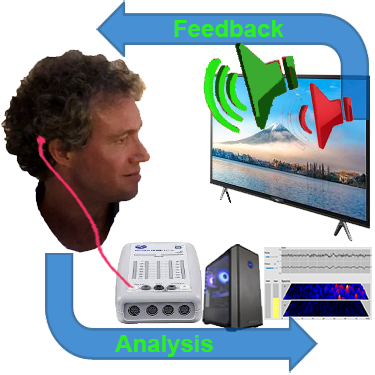
We use a movie of choice as the feedback mechanism – our conscious mind engages with the film, and feedback is delivered by small changes in volume or picture size.
Our pre-conscious mind adapts its behaviour to preserve the more comfortable volume and picture size, and learning occurs.
Volume changes are slight, not stop-start, and the process is enjoyable.
Key is that we are interested in the movie – our conscious mind is engaged with the content, which forms the reward, and our preconscious mind – without our conscious effort – changes its behaviour in response to the feedback.
A two hour training session allows us to do 90-110 minutes of neurofeedback training during which we can work on various brain sites.
This captures an entire ultradian rhythm cycle and corresponds to the approximate duration of feature film movies.
We can start with shorter sessions as appropriate, mainly with children.
Ideally, we do two or more sessions per week to start with.
We would expect to see responsiveness within the first few sessions and remap after twenty hours or about ten sessions.
Generally, we would expect to doing twenty sessions over two months, though this can vary substantially.
We can also accommodate intensives, where we do two sessions per day over a number of days, and have had good results with these.