Schizophrenia is a heterogeneous condition characterised by overactive internal content generation at the expense of synchrony with one’s environment. This can result in extreme withdrawal or psychosis, and is usually accompanied by a range of other mental health disorders such as ADHD, bipolar depression, OCD, insomnia and anxiety issues. Sensory integration can also be compromised, manifesting in hallucinations and other delusions.
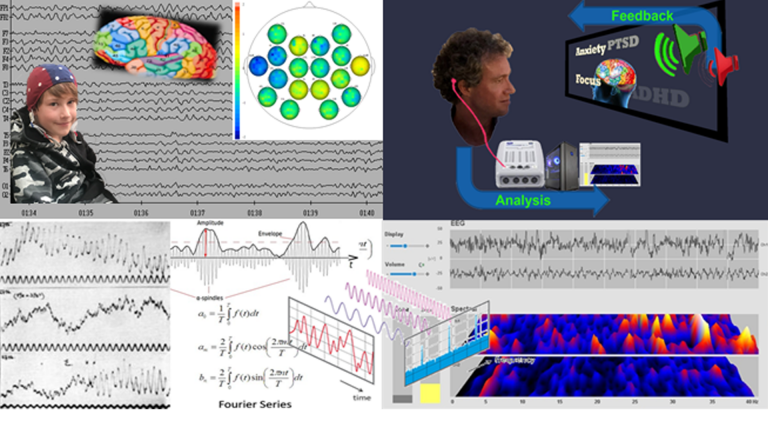
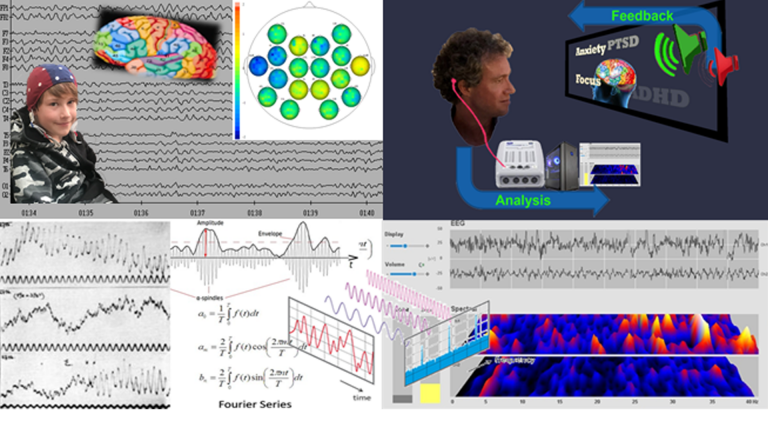
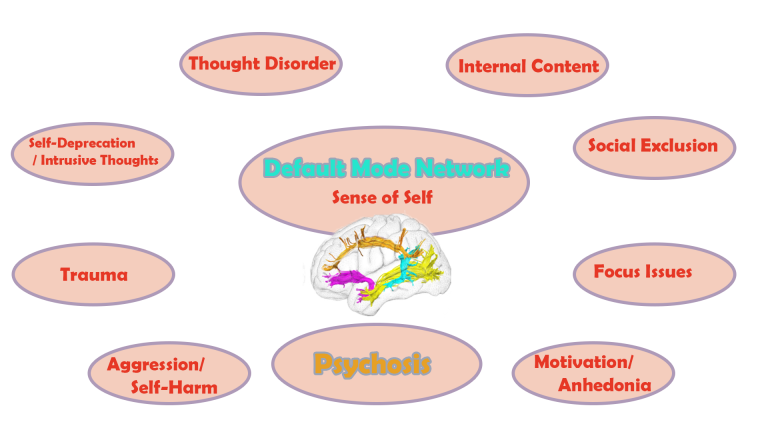
With a qEEG brain map, we can relate character traits and behaviour patterns to functional brain areas. Many symptoms have neural correlates that we can detect and train in a personalised way. The process is holistic in that we aim to restore the function of the Default Mode Network, the neural basis of self, and the integration of functional brain areas within their respective networks.
Neurofeedback training has been shown to be safe and effective for many symptoms, including hallucinations, and we have seen substantial progress per the Case Studies.
With Daniel Webster’s Neurofeedback, we can help the brain become more flexible, mature and integrated. This enables better social integration and resets trajectories, thus improving quality of life and promoting the full realisation of talents and potential.
The process is non-invasive, evidence-based, and enjoyable.
Daniel practices in London and Edinburgh, and is available for home visits internationally.

Overview of Daniel Webster's Neurofeedback for Schizophrenia

Changing Trajectories
Developmental expectations and trajectories are dampened by reduced social integration and cognitive inflexibility, and higher care or support requirements.
Early intervention can reduce this gap with peers and produce virtuous feedback loops.
Daniel Webster’s Neurofeedback produces transformational results in all age groups, as young as two.
Personalised Training
qEEG brain maps are a non-invasive way of analysing functional connectivity of over 40 brain areas, a measure of the health of the brain’s ‘wiring’, or relative contribution of each component.
Schizophrenia is a heterogeneous condition, requiring a personalised approach, bespoke to the person’s challenges.
Daniel Webster’s Neurofeedback is personalised brain training that is enjoyable – the person watches a movie of choice, the feedback is subtle (not stop-start) and training is passive, requiring only attention to the movie.
See here for more information on How it Works.
Personalised Training
qEEG brain maps are a non-invasive way of analysing functional connectivity of over 40 brain areas, a measure of the health of the brain’s ‘wiring’, or relative contribution of each component.
Schizophrenia is a heterogeneous condition, requiring a personalised approach, bespoke to the person’s challenges.
Daniel Webster’s Neurofeedback is personalised brain training that is enjoyable – the person watches a movie of choice, the feedback is subtle (not stop-start) and training is passive, requiring only attention to the movie.
See here for more information on How it Works.

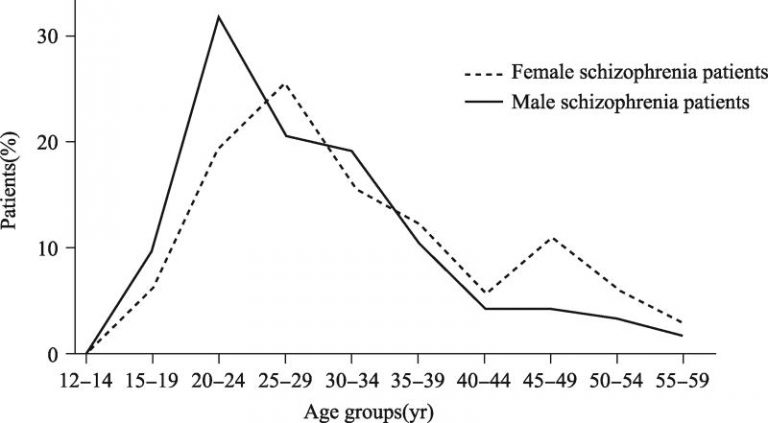
Schizophrenia is a developmental disorder that affects an estimated one percent of the population. Men are particularly prone to developing symptoms of schizophrenia in their late teens, while women are in their mid- to late twenties, and again susceptible during menopause.

Early symptoms involve increased social withdrawal, which is accompanied by the person’s substitution of external realities with an internal storyline of their own.
While in the extreme this can manifest in a complete detachment from the environment (‘florid’ states, or catatonia), it is most often a form of ‘augmented reality’ the person is experiencing.
Still interacting with others as much as necessary, the person’s perception is overlayered with internal content.

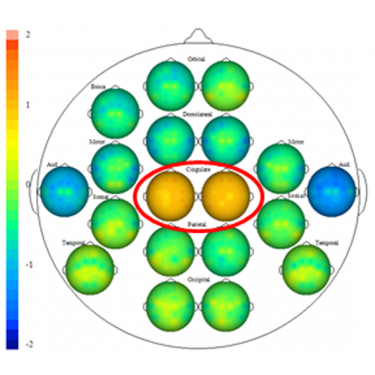
‘Thought disorder’ is a common diagnosis at this point. Areas in the temporal lobes provide the neural correlate for this phenomenon. We can determine vulnerability with a Kaiser Neuromap.
Neurofeedback training lets us strengthen the Default Mode Network, and we have seen the relevant site recover within seven sessions, though results may vary.
The client reports feeling ‘grounded’, ‘great’ and more settled in themselves, with better focus and presence of mind.

The internal content becomes no longer controllable with conscious awareness, especially when the person is in a physically exhausted or vulnerable state. In this case, the content can take on a negative, critical, even third-person dynamic.
‘Hearing Voices’ or ‘sparring with Dad’ (imagined authority) are frequent manifestations of when the internal dialogue becomes hostile.
Besides the effort of trying to disguise these internal processes to the outside world, the person is engaged in battling these competing perspectives, further fatiguing mind and self-esteem.

Sleep and focus deteriorate and a negative feedback cycle ensues with Insomnia, ADHD/ADD and bipolar depression frequently becoming ancillary diagnoses.
Intrusive thoughts result from of undigested experiences due to sleep deprivation, further fuelling the cycle.
All the while, the person is having to balance their internal turmoil with external interactions necessary to ensure their physical survival. Persistent paranoia and attribution of agency to illusions and hallucinations suffered can result in a delusion of being under constant observation and even persecution.

This projected imagination enlists emotions and sensory perceptions in a very ‘real’ way, and thus exceeds mere thought processes or ‘mental chatter’. The person becomes addicted to their own internal mental content as their reward circuitry embraces this simpler path, compared to ‘earning’ such rewards in their external interactions with their environment.

The internal imaginations become a habit to the extent that they are woven into the perceived reality – over 60% of sufferers are unaware of their condition or in active denial. Neurologically, the brain area where thoughts and hallucinations are believed to originate recruits the same neuronal network as that used to process external auditory stimuli (reality).

Mirror neurons remain active when in a self-referential state, which can be observed with a brain map, and are an indication of influences by perspectives other than their own. At times it becomes unable to distinguish fantasy from reality. This heightened activation towards external sensory influences, overpriming agency in the environment, can take multiple forms. With a Kaiser Neuromap, we can observe which type the person contends with:
– having the essence of another person in one’s head, such as from a recent conversation, or repeated interactions with someone of authority or emotional significance (‘imagined authority’); and/or
– excess consideration for our environment in general, such as increased concern for reputation; own agency competes with an internal perspective modelling judgment by the outside world at large (rather than by a specific person as above).

These phenomena are real and embedded in the neuronal intercommunication. Brain areas, often temporal lobe or with auditory involvement, are active to represent both own cortical resting rate, as well as accommodating perspectives other than one’s own. When the brain areas affected are in the visual or prefrontal domains, we see a propensity for hallucinations.

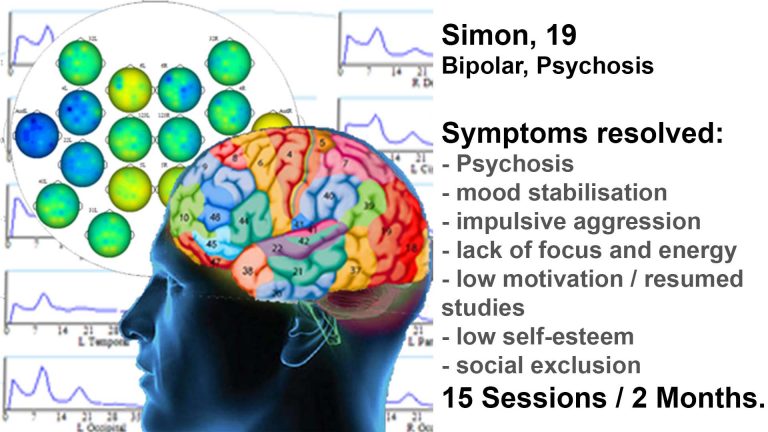
Schizophrenia is often accompanied by depressive or bipolar disorder, and can apply to people on the autism spectrum. Other comorbidities include PTSD, Obsessive-Compulsive Disorder (OCD), and General Anxiety Disorder.
The above definition excludes cases where the disturbance is attributable to substance abuse. Sufferers of the condition often turn to ‘self-medication’, which can intensify episodes. Schizophrenia is a developmental disorder, and as such doesn’t just remediate itself upon cessation of drink / drug / medication abuse.

Psychosis
Relational thinking is a necessary, yet not sufficient condition for psychosis.
Medication
A recent study also found that switching treatment-resistant patients onto clozapine found subsequent reduction in thalamic and hippocampal volume, enlargement of lateral ventricles (temporal lobe size decline) yet improved symptoms. Cortical thinning following 6-9 months of Clozapine treatment was also found despite symptom improvement, and causality between medication and anatomical change observations has yet to be established.
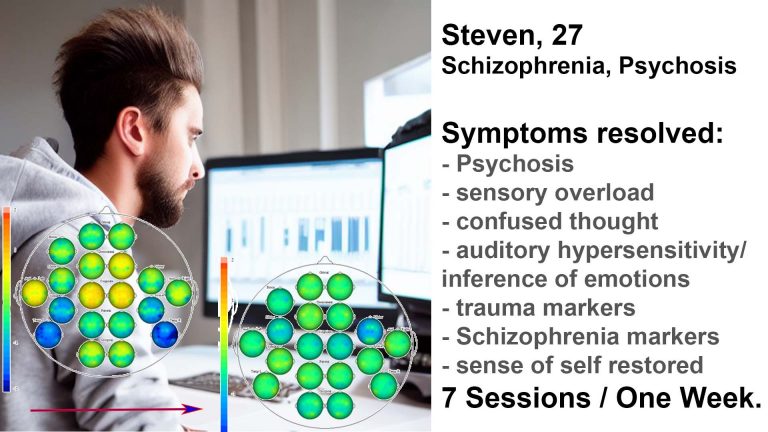
Case Studies:
Symptoms of Schizophrenia
Schizophrenia is a developmental disorder that affects an estimated one percent of the population. Men are particularly prone to developing symptoms of schizophrenia in their late teens, while women are in their mid- to late twenties, and again susceptible during menopause.
Early symptoms involve increased social withdrawal, which is accompanied by the person’s substitution of external realities with an internal storyline of their own. While in the extreme this can manifest in a complete detachment from the environment (‘florid’ states, or catatonia), it is most often a form of ‘augmented reality’ the person is experiencing. Still interacting with others as much as necessary, the person’s perception is overlayered with internal content.
‘Thought disorder’ is a common diagnosis at this point. Areas in the temporal lobes provide the neural correlate for this phenomenon. We can determine vulnerability with a Kaiser Neuromap. Neurofeedback training lets us strengthen the Default Mode Network, and we have seen the relevant site recover within seven sessions, though results may vary. The client reports feeling ‘grounded’, ‘great’ and more settled in themselves, with better focus and presence of mind.
The internal content becomes no longer controllable with conscious awareness, especially when the person is in a physically exhausted or vulnerable state. In this case, the content can take on a negative, critical, even third-person dynamic. ‘Hearing Voices’ or ‘sparring with Dad’ (imagined authority) are frequent manifestations of when the internal dialogue becomes hostile. Besides the effort of trying to disguise these internal processes to the outside world, the person is engaged in battling these voices, further fatiguing mind and self-esteem.
Sleep and focus deteriorate and a negative feedback cycle ensues with Insomnia, ADHD/ADD and bipolar depression frequently becoming ancillary diagnoses. All the while, the person is having to balance their internal turmoil with external interactions necessary to ensure their physical survival. Persistent paranoia and attribution of agency to illusions and hallucinations suffered can result in a delusion of being under constant observation and even persecution.
Both the ‘Voices’ phenomenon and hypervigilance have neural correlates that we can detect with a Kaiser Neuromap. We can then train these accordingly with Default Network Training, an advanced form of neurofeedback devised by one of the founders of the field, David Kaiser PhD.
This projected imagination enlists emotions and sensory perceptions in a very ‘real’ way, and thus exceeds mere thought processes or ‘mental chatter’. The person becomes addicted to their own internal mental content as their reward circuitry embraces this simpler path, compared to ‘earning’ such rewards in their external interactions with their environment.
The internal imaginations become a habit to the extent that they are woven into the perceived reality – over 60% of sufferers are unaware of their condition or in active denial. Neurologically, the brain area where thoughts and hallucinations are believed to originate recruits the same neuronal network as that used to process external auditory stimuli (reality).
Mirror neurons remain active when in a self-referential state, which can be observed with a brain map, and are an indication of influences by perspectives other than their own. At times it becomes unable to distinguish fantasy from reality. This heightened activation towards external sensory influences, overpriming agency in the environment, can take multiple forms. With a Kaiser Neuromap, we can observe which type the person contends with:
– having the essence of another person in one’s head, such as from a recent conversation, or repeated interactions with someone of authority or emotional significance (‘imagined authority’); and/or
– excess consideration for our environment in general, such as increased concern for reputation; own agency competes with an internal perspective modelling judgment by the outside world at large (rather than by a specific person as above).
These phenomena are real and embedded in the neuronal intercommunication. Brain areas, often temporal lobe or with auditory involvement, are active to represent both own cortical resting rate, as well as accommodating perspectives other than one’s own. When the brain areas affected are in the visual or prefrontal domains, we see a propensity for hallucinations.
Schizophrenia is often accompanied by depressive or bipolar disorder, and can apply to people on the autism spectrum. Other comorbidities include PTSD, Obsessive-Compulsive Disorder (OCD), and General Anxiety Disorder.
The above definition excludes cases where the disturbance is attributable to substance abuse. Sufferers of the condition often turn to ‘self-medication’, which can intensify episodes. Schizophrenia is a developmental disorder, and as such doesn’t just remediate itself upon cessation of drink / drug / medication abuse.
Note that more than half of all diagnosed SSD sufferers do not acknowledge their condition, and as such it appears that many diagnoses make the external, subjective assertion of the existence of hallucinations or incoherence. On the other hand, distinguishing ‘normal’ internal dialogue / mental chatter from excessive internal content generation can be difficult for less interoceptive individuals, who might not even be aware of their difference.
The first signs of this development are often missed, as they occur in a naturally transformational period such as puberty, or menopause. The mind starts becoming addicted to its own content, thus diverting resources from the social interactions that are necessary during nascent personality building.
Cannabis / Marijuana use is often linked to the development of Schizophrenia Spectrum Disorder. Its frequent concurrent use has prompted publication of over 1,500 studies, with divergent findings regarding causality and exacerbation of symptoms. Cannabis use doubles the risk of developing psychosis in vulnerable people, particularly during adolescence, where it can impair growth.
The incidence of schizophrenia is higher in urban settings, having doubled in south-east London over the past three decades.
Schizophrenia is characterised by the DSM-5 as follows:
– Two or more of the following Characteristic Symptoms, present for a significant portion of time during a one-month period:
+ Delusions;
+ Hallucinations;
+ Disorganised Speech (e.g. frequent derailment or incoherence);
+ Grossly disorganised or catatonic behaviour;
+ Negative Symptoms (i.e. diminished emotional expression or avolition)
– Social / Occupational Dysfunction, i.e. level of functioning in one or more major areas (work, interpersonal relations, self-care) markedly below the level achieved before onset, or failure to achieve expected levels of interpersonal, academic or occupational functioning for a given age-group
– Duration of disturbance lasting for at least six months, of which the above symptoms persist for at least one month
Neurofeedback for Schizophrenia
In Schizophrenia, the formation of a neural basis for a ‘self’, the Default Mode Network, is impaired, as is its ability to anti-correlate with the Central Executive Network. Key nodes of these networks are often dysrhythmic, impacting the ability to self-sooth and self-nurture.
Thought disorders, delusions or hallucinations are signs of not engaging sufficiently with the outside world. These have neural correlates which we can detect with a Kaiser Neuromap and then train with neurofeedback.
Many other pathologies ensue, including trauma, mood dysregulation, sleep and focus issues, and other personality disorders are at risk of developing as the social brain breaks down.
With neurofeedback, we aim to restore social functionality, launching the person back into a virtuous cycle of affirmation and productivity with others.
Daniel Webster has done week(s)-long intensives with clients, where substantial progress was made in reducing psychosis and trauma symptoms. This was ascertainable with before and after Kaiser Neuromaps, corroborating positive functional connectivity changes. These were confirmed cognitively by the clients and their families. Daniel has extensive experience working with sufferers of Schizophrenia in clinical and care settings, as well as in post-psychosis recovery and rehabilitation.
Neurofeedback is a form of complementary therapy and works alongside medication and psychotherapy, as well as calm-inducing approaches aimed at re-socialisation and maximising of interpersonal function.
Schizophrenia is a manageable disorder. There are usually a number of comorbidities, such as mood regulation, sleep issues, distractibility, anxiety / paranoia, self-harm and rage, and social anxiety. Each of these can be addressed with neurofeedback training.
Our brain has over 40 distinct processing areas, interpreting stimulus from our senses to provide us with an awareness of our surroundings, and the ability to interact with it pro-socially. Mental Health issues arise when one or more brain areas are dysrhythmic.
With a Kaiser Neuromap, we can assess which areas are stressed. We can then train these areas with neurofeedback. This is an enjoyable process whereby our conscious mind is focussed on a movie, while our preconscious mind registers the feedback – given through short, slight drops in loudness – and corrects its behaviour to restore the more comfortable volume. Learning occurs, and is exercised through repetition to produce lasting effects.
Kaiser Neuromap – based Personalised Brain Training respects individuality and tailors a therapy approach in a holistic way.
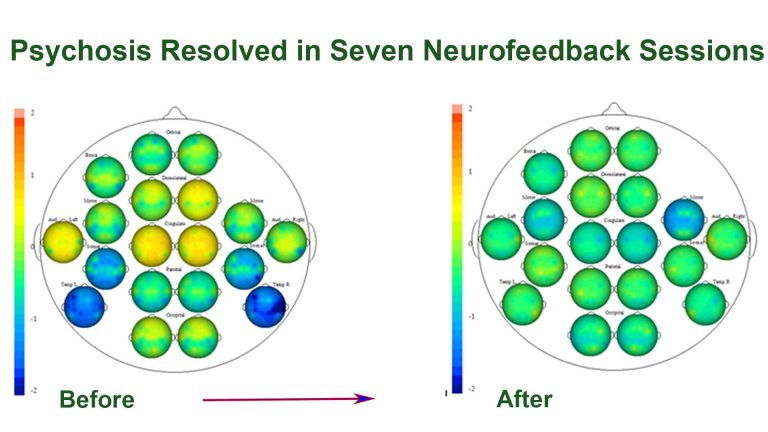
A one-week intensive neurofeedback training course produced the pictured result. We were able to stabilise brain function by eliminating crucial psychosis and trauma markers.
Cognitively, this manifested in a new sense of calm, groundedness and self-confidence. Sensory overload, auditory sensitivity and thought confusion were substantially reduced. Parents of the client noted significant calming, agreeability and consideration. This is a strong change that now needs to consolidate, by giving the client space and time as well as support for productive habit forming (e.g. self-awareness exercises, physical training and an opportunity to redefine themselves).
We did seven two-hour neurofeedback sessions in six days, in London.
Neurofeedback Training can help address specific schizophrenia symptoms and comorbidities including:
– Default Mode Network functionality and psychosis
– ‘Voices’, auditory, visual and kynaesthetic delusions
– Paranoia and Anxiety
– Thought disorder
– Sleep disorders
– Mood disorders and emotional self-regulation, including depression / bipolar disorder
– Attention switching and focus
– Sense of self
– Self / Other distinction
– Shared authority and societal rules / conventions
– Borderline Personality Disorder
– Obsessive Compulsive Disorder (OCD)
– Addiction and vulnerability to substance misuse
– Aggression and social invasiveness
– Suicidal ideation / self-harm
Neurology of Schizophrenia
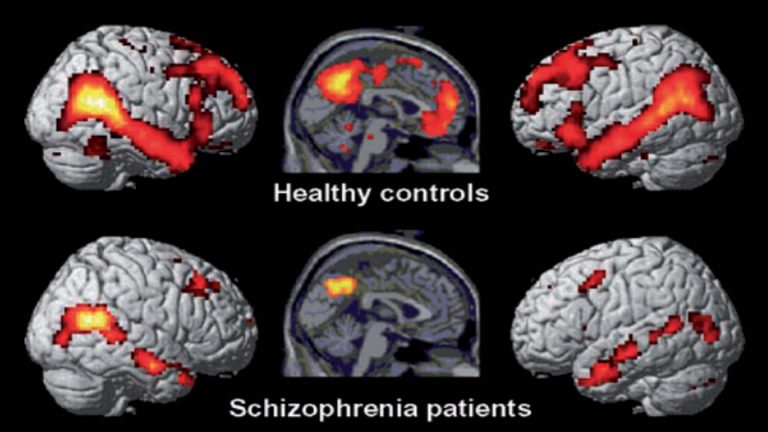
Looking into the brain by means of an fMRI scan, the following differences in activation have been found compared to healthy controls. As this is an observation of patients in a task-neutral, resting state, the differences in activation reflect the strength of the Default Mode Network (DMN) .
The DMN is a network of neural hubs that are active when we are in a self-referential state – when there are no external demands on the brain. Interestingly, the brain consumes about one-fifth (20%) of all energy used by our entire organism, and during resting state, the brain uses only 5% less energy than when ‘active’ in a task-positive way. (The notion that we only use a fraction of our brain is a myth borne out of the observation that birds only loose their ability to fly when 90% of their brain is removed.)
The research on the DMN during the last two decades further demonstrates that we very much rely on our brain functioning during resting state: we don’t go into ‘shut-down’ during sleep and relaxation, but are virtually as active when doing nothing as when we are actively thinking.
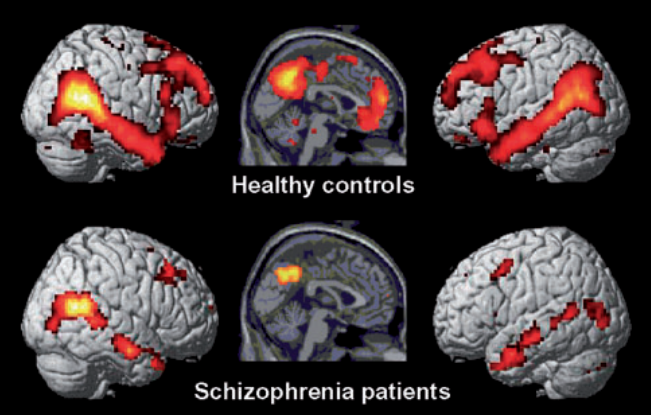
In Schizophrenia, the Default Mode Network is substantially weakened. The maternal neural hub is dysrhythmic, while the paternal hub’s activity is hardly identifiable in the illustration above. Attention switching ability is impaired, as is the hub responsible for attributing agency to observations, thus resulting in delusions. Sources of anxiety and mood disorder are also identifiable as is the susceptibility to substance abuse and addictive behaviour. With one in three sufferers of Auditory Verbal Hallucinations (AVH) resistant to conventional interventions (medication), research into alternative approaches has increased in recent years. Neurofeedback training of the arcuate fasciculus has been shown to provide significant improvement in AVH and reduced symptoms.
Hearing ‘Voices’ and other sensory delusions are a function of excess neural activity, giving rise to the existence of another internal perspective other than one’s own. This overexcitement resembles hyper-vigilance as the nervous system is over-primed to external stimuli. The secondary auditory processing region in the brain – most often associated with schizophrenia and auditory hallucinations (BA21L) – accommodates both the internal acoustic information and external sounds. This could be one of the reasons sufferers of the disorder are frequently unaware or in denial of their affliction.
‘Hearing Voices’, or auditory hallucinations, can take many forms. Some sufferers experience a mainly benign ‘soundtrack’ or musical accompaniment in their head. Others hear a realistic, internal, critical commentary, heightening their sense of feeling watched and struggling with an imagined authority whose ferocity increases as the person tires physically and mentally. The strain on self-esteem is both direct, due to its critical nature, and secondary in that the constant experience diverts the person from the moment and other self-reflective, self-soothing thoughts. A search for both confidence and numbing often finds a self-destructive drug-cycle that exacerbates the issue of lacking social engagement.
Differences between the brains of Schizophrenia Spectrum Disorder sufferers and Healthy Controls have been documented in numerous studies. These include lower Gray and White Matter Volume (GMV / WMV) in left temporal and frontal lobes; excess GMV in the basal ganglia (correlating with positive symptom severity); reduced density of key fasciculae (long distance white matter tracts); loss of GMV, particularly in males past age 35 and prefrontal glial cell loss.
White matter tracts are particularly – adversely – affected in schizophrenia. More than 50% of cortico-cortical and cortico-thalamic connections were shown to be affected, in particular connections between key neural hubs of the default mode network. Reduction in FA (fractional anisotropy, a proxy for functional connectivity) affected 40% of cerebral white matter volume (234ml, or one US cup) in this study. This finding is particularly interesting, as neurofeedback training has been shown to be able to strengthen white matter tracts.
A recent study also found that switching treatment-resistant patients onto clozapine found subsequent reduction in thalamic and hippocampal volume, enlargement of lateral ventricles (temporal lobe size decline) yet improved symptoms. Cortical thinning following 6-9 months of Clozapine treatment was also found despite symptom improvement, and causality between medication and anatomical change observations has yet to be established.
Finding neuromarkers specific to Schizophrenia is a challenge created by the relatively broad definition of the disorder (which serves as the criterium for participant selection in studies), and the commonality of comorbidities such as anxiety, depression and other mood and personality disorders. The benefit of qEEG-brain map based Default Network Training is that we can form a personalised brain training plan that recognises the individuality of each brain.
Causes of Schizophrenia
Schizophrenia is a spectrum disorder, meaning that severity, onset and manifestation of symptoms can vary substantially. It’s more modest expressions can still produce symptoms such as borderline personality disorder (BPD) and/or Dissociative Identity Disorder (DID). High performing schizophrenics can effectively mask their symptoms to maintain a functional appearance at work or around family. The lack of maturation or development of a true ‘self’ however undermines efforts to gain true emotional satisfaction and fulfilment. This has a disintegrative effect that tends to become more pronounced with age. It is not unusual to see the construct of an outward appearance to fall apart with middle age. This form of non-florid schizophrenia, which would probably struggle to fit into the DSM-5 definition below, partly because the person would likely not classify their internal content as ‘hallucinations’. Some such sufferers are able to turn their internal activity into a creative expression in the form of literature, art or science.
A genetic predisposition to schizophrenia can be set off by exclusion from the external environment. Migration, that is, higher exposure to social adversity, has been found to substantially increase the risk of developing schizophrenia. Cannabis use in adolescents has been linked to schizophrenia since the 1980s, and it’s ability to stimulate internal content generation could be one reason for the high rate of use among persons on the schizophrenia spectrum.
Schizophrenia and its comorbidities can be debilitating and leading a fulfilling and productive life a challenge. Life expectancy and quality are reduced by this spectrum condition. Negative symptoms of social withdrawal and anhedonia emerge usually during mid-life. Yet many creative minds have shared this struggle.
A genetic predisposition to schizophrenia can be set off by exclusion from the external environment. Migration, that is, higher exposure to social adversity, has been found to substantially increase the risk of developing schizophrenia. Cannabis use in adolescents has been linked to schizophrenia since the 1980s, and it’s ability to stimulate internal content generation could be one reason for the high rate of use among persons on the schizophrenia spectrum.
Psychosis
A feature of psychosis is a state of mind where all sensory stimulus is interpreted as being directed to oneself.
While it is natural for infants and children to interpret the world this way, we grow out of this mode between the ages of 3-5. We can assist this important maturation step with neurofeedback training.
As we mature, we start to learn that not everything that’s happening in the world is directed at ourselves.
Feeling as if everything is directed at us results in anxiety and / or deep depression, and clouds our interactions with others.
It also reduces our ability to take on other perspectives, consider different views and be accommodating of others’ stances. This reduces people’s self-awareness and thus insight into the need for change and improvement, providing another obstacle to betterment.
Shocks, such as trauma, drug use (in particular, cannabis and cocaine) and isolation (such as lockdowns) can cause us to revert into this child-like state, without us noticing.
Psychosis is a state that can occur, and recur, in persons diagnosed with Schizophrenia, Bipolar Disorder, Trauma and neurodegenerative conditions. Note however that it is not a necessary condition for any of these.
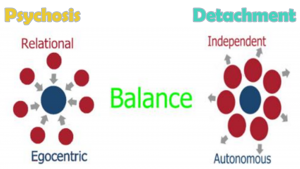
Psychosis can be seen as a state opposite to detachment. We want a healthy sense of distance, and thus a happy medium, to be able to take on different perspectives, and not feel as though everything is always directed at us, when quite possibly, it isn’t.
With a Kaiser Neuromap, we can identify whether someone is prone to relational thinking as defined above.
Research confirms this phenomenon in fMRI studies.
Hallucinations
Psychosis can be seen as a state opposite to detachment. We want a healthy sense of distance, and thus a happy medium, to be able to take on different perspectives, and not feel as though everything is always directed at us, when quite possibly, it isn’t.
With a Kaiser Neuromap, we can identify whether someone is prone to relational thinking as defined above.
Research confirms this phenomenon in fMRI studies.
Besides florid and sometimes unstructured thought processes, some people experience strong internal dialogue. The intensity varies on a spectrum, from distracting, intrusive thoughts, to detached, and often commanding, ‘voices’ that are attributed to external agency. Depending on mood and the person’s stability in terms of sense of self, these distractions can become negative, critical and oppressive, to the extent they overpower internal agency and exert control.
Some people find engagement with these thoughts soothing in that they gain a sense of control. This process is often fuelled by alcohol or drugs, and can result in ‘sessions’ that last until physical exertion. Others are overpowered gradually, and succumb to numbing and anhedonia.
With a Kaiser Neuromap, we can detect vulnerability to this phenomenon. We can even localise it, and understand whether only auditory and executive areas are affected, or whether visual and tactile hallucinations are possible. qEEG analysis lets us identify neuromarkers for hallucinations, ‘voices’ and other such interference.
With neurofeedback training, we have had success in attenuating these distractors, thus quietening the mind in an organic manner. The result is a calmer, more self-assured person.
One in three Schizophrenia sufferers experience pharmacology-resistant auditory verbal hallucinations (AVH); in 30% of cases antipsychotic medication has little or no effect. Neurofeedback training has been shown to produce significant results in this population, reducing auditory verbal hallucinations.
Voices, delusions and hallucinations do not have to be negative in nature. Our general sense of mental well-being has a strong influence on whether these are hostile or more manageable – even musical.
Personalised Brain Training helps us work on our core sense of self.
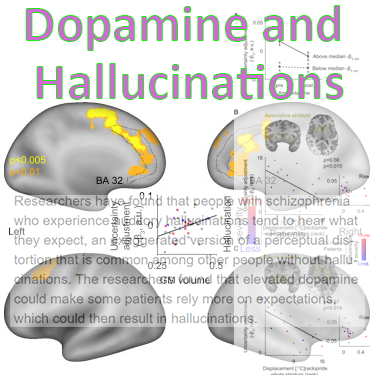
Hallucinations in Schizophrenia and other pathologies have been found to be linked to the dopamine system. People who experience auditory hallucinations tend to hear what they expect. This is often inked to intrusive, self-critical thoughts or emotions.
Researchers have found that elevated dopamine levels can result in the person relying more on expectations, which in turn can result in hallucinations.
In general, the process of sensory perception is an optimal combination of prior expectations and new sensory input. If prior expectations are given to much weight in this combination process – which is constantly happening as we take in the world – perceptual distortions can occur, such as illusions and hallucinations. Those with hallucinations and other symptoms of psychosis are known to have elevated dopamine levels, and research has now established a link.
Hearing voices; self-critical thoughts taking on third person dimensions, are a result of mirror neurons firing even when the person is in a state of rest. We can detect vulnerability to this with a Kaiser Neuromap, and train this accordingly with neurofeedback. We have treated even rarer visual and tactile hallucinations this way with Personalised Brain Training.
Thalamo-cortical connections play a part in auditory hallucinations too.
Famous People with Schizophrenia

– John Nash Jr. – Mathematician, Nobel Laureate, subject of the movie “A Beautiful Mind”
– Albert Einstein, Bertrand Russell – both had schizophrenic sons
– James Joyce – had a schizophrenic daughter
– Zelda Fitzgerald, F. Scott Fitzgerald’s wife
– Jack Kerouac
– [J.D. Salinger’s Holden Caulfield in “The Catcher in the Rye”]
– Syd Barrett of Pink Floyd; drummer Jim Gordon; Peter Green of Fleetwood Mac; jazz musicians Buddy Bolden and Tom Harrell; Skip Spence of Jefferson Airplane; Joey Ramone from The Ramones
– Actresses Veronica Lake, Gene Tierney, Bettie Page
– Darrell Hammond of Saturday Night Live
– Photographer Vivian Maier, subject of the documentary Finding Vivian Maier
– Lionel Aldridge, NFL player; became homeless before diagnosis and turned to mental health advocacy in later years
– Bobby Fischer, World Champion Chess player
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.