Neurofeedback for Rehabilitation
Daniel Webster’s Neurofeedback has produced strong results in neurorehabilitation.
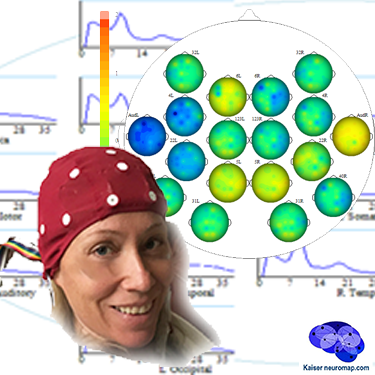
A qEEG brain map lets us detect issues with functional connectivity between brain areas, thus complementing MRI and other scans.
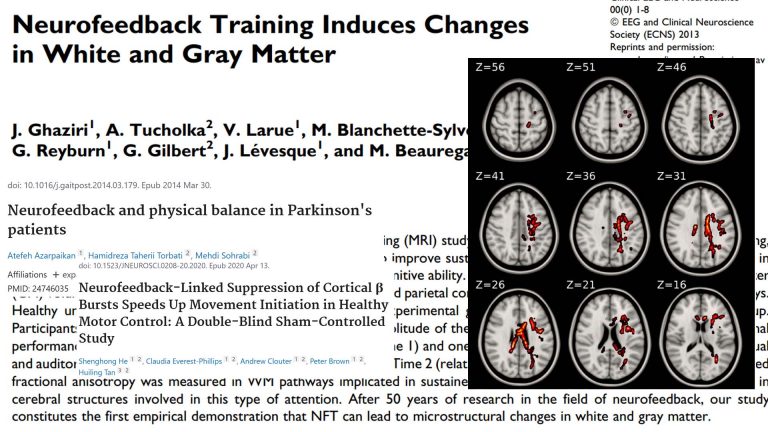
Neurofeedback has been shown to make positive structural improvements to the brain, improving myelination.
Symptom reduction, improved movement and sensory integration are evidence-based.
Secondary mental health issues, such as trauma, mood control, anxieties, sleep issues and impulsive aggression can also be addressed with neurofeedback training.
Stroke
Neurofeedback is an effective complementary rehabilitation measure in post-stroke recovery.
See Case Study here.
Concussion / TBI

With a brain map, we can identify post-concussion head trauma.
Neurofeedback training is an effective complementary recovery measure in rehabilitation.
PoTS
Postural Tachycardia Syndrome (PoTS) has been treated effectively within three months in this neurofeedback Case Study.
Neurofeedback and Stroke
The following account of the recovery of a Stroke patient illustrates the potential efficacy of neurofeedback for Stroke / TBI. For Research on neurofeedback and Stroke / TBI see here.
Claire (name changed) is a 48-year old female who is three years post-thalamic CVA (ruptured aneurysm). In particular, her physical symptoms included severe muscle contractures in her wrist and elbows leading to impaired movement, as well as being wheel-chair bound.
After two neurofeedback sessions, she got her wrist and elbow released.
Claire was getting active elbow extension and shoulder flexion after five sessions. Pain was also resolved in her hand, which had been a major issue previously.
Functionally, she achieved improved independence in dressing skills, required only minimal assistance with bathing, and was able to walk with a cane.
After thirty neurofeedback sessions, Claire started walking without her cane.
Significant improvements (over 50%) included:
– Working memory, chronic aching pain, attention deficit
– night sweats, vertigo and hot flashes
– body awareness, balance, fine motor coordination, muscle spasticity, reflux and chronic nerve pain
– paranoia
Note that this is a subjective account from a therapist and a causal relationship between training and improvements is not proven.
Neuroplasticity is the process by which neurons form new synapses, or connections, and this ability is highly adaptive during both health and disease. Neurofeedback has been shown to promote this process.
Intra-day fluctuations in performance and function in persons affected by a neurodegenerative condition imply that neuronal loss (or gain) is not the only mechanism at work. The connectivity of neurons – their ability to form networks which contribute to memory and thought formation and ultimately our sense of self – is variable.
We also believe that maintining client functionality in the optimum range can help shape more positive trajectories.
Neurofeedback and Concussion / TBI
There are neuromarkers for concussion / mild Traumatic Brain Injury (mTBI). With a brain map, we can detect these.
Functional connectivity between brain areas is also altered post injury. Compensatory mechanisms often result in character changes, which have neural correlates. We can detect these, and train them accordingly.
qEEG provides a complementary view of post-injury brain changes, many of which are not visible in MRI or other scans. This can also provide a basis for further investigation, as structural changes can be missed on these scans.
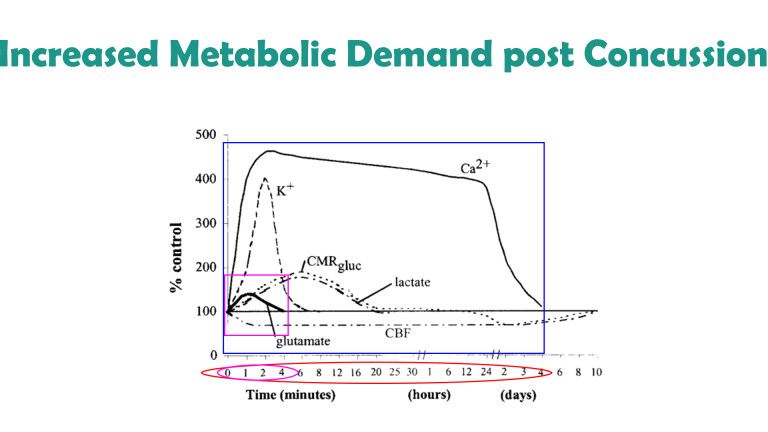
Neurofeedback training lets us aid recovery. Post impact, the brain experiences increased metabolic demand as a result of various imbalances. This happens against a background of decreased cerebral blood flow. This strain can last for days, during which the brain is particularly vulnerable to further insult. With neurofeedback, we can detect signs of injury (while not providing diagnosis), and promote effective ‘rewiring’, or functional connectivity during the rehabilitation process.
Mentally, trauma-like symptoms often appear, as well as memory issues and heightened emotional reactivity. The person can become more impulsive, aggressive and activated; and/or switch rapidly to withdrawal, apprehension and disinterest in social involvement. Attention switching, focus and mood control can be impacted, and we can detect neuromarkers for these with Daniel Webster’s qEEG brain map. Neurofeedback lets us address these ‘secondary’ issues in an evidence-based, non-invasive, medication-free manner that is enjoyable and has produced strong and lasting results.
There are various phases to recovery, and we want to assist the brain in re-establishing homeostasis at each stage to prevent permanent damage. Repeated injury will lead to phenomena such as CTE, which are noticeable in middle and later age, and is linked to heightened susceptibility to Alzheimer’s Disease.
This is a non-invasive, medication-free approach. See below for research.
The process is holistic – a brain map shows us other vulnerabilities, which we also train. In athletes, this includes:
– focus and planning
– motivation and persistence
– resilience: approach to unexpected outcomes, repurposing impulsive aggression
– ability to self-soothe
– control of physiological arousal (staying calmer, calming down quicker)
– sleep, both onset and quality; important for learning, consolidation and general mental health
– various anxieties
– mood control.
Neurofeedback and PoTS
Postural Tachycardia Syndrome (PoTS) was first described in the 1940s, refined in 1993 and finally received a specific diagnostic code in October 2022. It is characterised by exercise intolerance and near syncope upon standing upright, elevated pulse (tachycardia) by 30-40bpm within 10 minutes of standing up, fatigue, anxiety and light-headedness. Often misdiagnosed as chronic anxiety or panic disorder, the group of symptoms comprised by PoTS has a biomarker and increasingly considered an autoimmune disorder, rather than only autonomic nervous system dysfunction. Specifically, increased levels of cytokines and chemokines characteristic of an innate immune condition were found, similar to autoimmune diseases like multiple sclerosis, psoriasis, type-1 diabetes, rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
The condition affects females five times more frequently than males, mainly between 15-25 years of age, with over one million affected in the US alone. PoTS symptoms can persist for years, though half of patients find that orthostatic symptoms and functional impairment subside within five years, and of thost most within 1-2 years. It is estimated that 2-14% of Covid sufferers go on to develop PoTS, while 30% of long Covid patients, especially women, meet the diagnostic criteria.
A client presenting with PoTS like symptoms, recovered within three months of starting neurofeedback training, to the extent that the tachycardia was fully under control and anxieties had subsided substantially. Notably, physical symptoms became manageable, from being previously incapacitating, in a relatively short period of time. This result is encouraging, especially with regard to the speed and extent of recovery, and neurofeedback has been shown to be effective for anxiety. Also, in this person, other neurological issues could be detected with qEEG.
Research on Neurofeedback for Rehabilitation
– Alpha-Theta neurofeedback training has a “beneficial effect on symptom reduction as well as perceived stress. It also has a beneficial effect on levels of serum cortisol” involving a significant reduction during acute recovery
– neurofeedback training was shown to be effective with Postconcussion Syndrome (PCS)
– efficaceous treatment for chronic posttraumatic headache sustained in military service
– neurofeedback therapy showed significant changes in structural and functional connectivity in young TBI patients, with cognitive scores and concussion symptoms improving significantly
– neurofeedback is shown to be an effective intervention for auditory memory
– deemed “probably an excellent complementary technique” that produced clear benefits in divided and sustained attention, visuospatial skills and the processing speed of motor-dependent tasks in persons with severe TBI
– beneficial outcomes in upper limb stroke rehabilitation
– neurofeedback training can lead to a learned modulation of brain signals with associated changes at both neural and behavioural level
– modulation of premotor cortex and associated motor control areas can be achieved with neurofeedback training
– improvements in TBI / PTSD in Vietnam Veterans across domains of cognition, pain, sleep, fatigue, mood/emotion, PTSD symptoms and overall activity levels
– patients report improvement in a wide range of neuropsychiatric symptoms in TBI following neurofeedback training
– result of 40 neurofeedback sessions included significant improvements in several motor tasks
Secondary Mental Health Effects of TBI / Stroke
As the brain’s functional connectivity is impacted by physical trauma, changes in character can occur. These include aspects of self-sustainability, such as mood regulation, sleep and anxieties; and extend to sense of self, re-assessment of social and personal boundaries, impulsive aggression and rage, focus and productivity as well as sense of emotional security.
With neurofeedback training we can address these issues in a personalised manner, based on a Kaiser Neuromap. The person feels more comfortable and optimistic about their progress as we restore hope and sense of accomplishment.
Comorbid mental health issues, such as anxiety, depression, aggression, PTSD and mood imbalances can be addressed directly with neurofeedback. We strengthen sense of self and improve emotional regulation.
Chronic Pain is another application for neurofeedback, where studies have demonstrated its efficacy.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
The Process Explained
Step 1: Brain Map
A qEEG recording takes about 45minutes for a 20 minute recording.
A cap with 19 sensors is is fitted to our head and gels inserted to ensure connectivity. The sensors only read – there is a tiny voltage on the surface of our head that these pick up. The gels are easily washed out later. This is also the last time we wear the cap (until a remap after ten sessions); training is done with single sensors.
We analyse the data with Kaiser Neuromap software which gives us a unique view into character traits and vulnerabilities.
Findings are presented in a separate one-hour conversation where we discuss the key elements.
Step 2: Neurofeedback
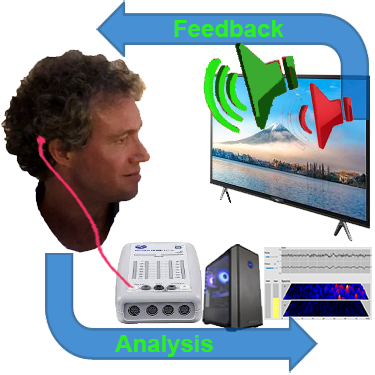
We use a movie of choice as the feedback mechanism – our conscious mind engages with the film, and feedback is delivered by small changes in volume or picture size.
Our pre-conscious mind adapts its behaviour to preserve the more comfortable volume and picture size, and learning occurs.
Volume changes are slight, not stop-start, and the process is enjoyable.
Key is that we are interested in the movie – our conscious mind is engaged with the content, which forms the reward, and our preconscious mind – without our conscious effort – changes its behaviour in response to the feedback.
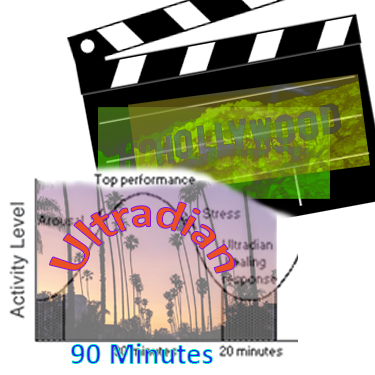
A two hour training session allows us to do 90-110 minutes of neurofeedback training during which we can work on various brain sites.
This captures an entire ultradian rhythm cycle and corresponds to the approximate duration of feature film movies.
We can start with shorter sessions as appropriate, mainly with children.
Ideally, we do two or more sessions per week to start with.
We would expect to see responsiveness within the first few sessions and remap after twenty hours or about ten sessions.
Generally, we would expect to doing twenty sessions over two months, though this can vary substantially.
We can also accommodate intensives, where we do two sessions per day over a number of days, and have had good results with these.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
Brain Maps and Personalised Brain Training Explained
Personalised Brain Training with Neurofeedback
Neurofeedback lets us train dysrythmic brain areas. With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, short and instantaneously.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the movie; the training process is passive in this sense.
The drop in volume is subtle, so we continue to understand the flow of the movie. No current or electrical stimulation is fed to the brain; sensors simply read brainwaves and the feedback is purely audio-visual.
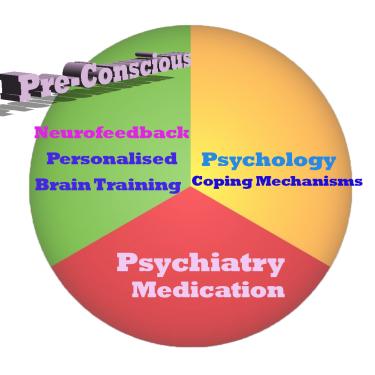
Neurofeedback trains our Pre-Conscious Mind
Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
This equips us with the ability to live in the moment and attain our potential (if we have to resort to conscious control, we are not living in the moment).
We take a holistic approach to healthy brain self-regulation, rather than categorisation or diagnosis.
Personalised Brain Training is an advanced qEEG brain map-based approach to neurofeedback training developed by the founders of the field. Taking Othmer Method / ILF training methods further, it employs Default Network Training protocols as developed by David Kaiser.
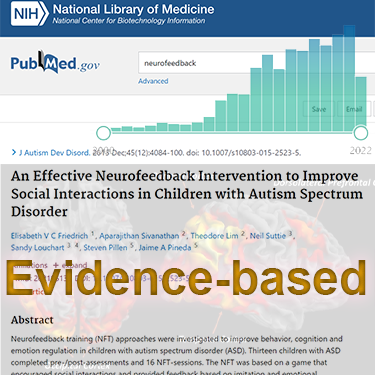
Neurofeedback is Evidence-based
Neurofeedback training is an evidence-based complementary therapy. Its efficacy was first demonstrated some 50 years ago, and with advances in technology, training protocols have become more efficient and the feedback method – watching movies – thoroughly enjoyable.
Neurofeedback is evidence-based. It’s first application was discovered in 1971 when it was used to resolve intractable epilepsy.
There are over 2,000 peer-reviewed research reports on PubMed demonstrating efficacy across a number of pathologies.
In the US, it is an accepted complementary treatment for many challenges.