Neurofeedback Restores Mood Control and Sense of Self
Neurofeedback training has been found to significantly help 80% of people with depression by aiming to restore motivation and mood control, improving sleep and focus, and reducing anxiety. We can also equip the brain to deal with trauma and intrusive thoughts, and take on a positive attitude to “get over it”. This helps us move forward with an optimistic mindset, free from self-doubt.
The positive effects of neurofeedback training have been shown to be lasting.
Neurofeedback is non-invasive and medication-free.
Depression is like a dark cloud hanging over our head. Shackled by our negative emotions, drive disappears, and everything becomes an effort. We are having to divert valuable energy resources to the mere concept of coping, and become lost without perspective. Drained of confidence and optimism, our social functioning is impaired and we enter a negative cycle that is ever more difficult to escape, while our physical well-being is affected. Achievement and optimism seem faint ideals, and we feel trapped. An extended state of anhedonia can ensue, further undermining our sense of self. We can also find ourselves in a cycle, where good days are marred by anxiety that we fall back into our previous state again. Overcoming depression is a challenge that can give us great strength and help us come out stronger.
We find there are several key aspects to overcoming depression:
– having a healthy sense of self, feeling grounded and part of something bigger
– living in the moment: Being There, rather than ruminating about the past or worrying about the future; an optimistic mindset that lets us see the best and get the most out of every situation in a flexible and constructive manner
– regaining functionality: restoring focus and motivation, being able to complete projects and gain a sense of achievement; losing anxieties and sleep issues; optimising mood control; and creating positive social interactions and relationship dynamics
To successfully overcome depression, we want to (re-)establish ourselves and regain a positive trajectory, shaping our environment in a way that becomes self-reinforcing. Neurofeedback can help us along this rewarding path.
Depression is like a cloud that’s inside the head, invisible to others, which absorbs our ability to engage with the outside world to the fullest. Motivation drops, focus, sleep and diet suffer, and mood can swing with bipolar disorder which affects one in five people with depression.
Bipolar Disorder is estimated to affect over 4% of adults at some point in their lives, compared to 12% for unipolar depression. More than two-thirds of BP sufferers are misdiagnosed initially, and one-third remain misdiagnosed for ten years or more.
Sadly, BD is strongly linked to suicide risk, with 20-60% attempting this during their lifetime and up to 19% succeeding, thus accounting for up to one in seven suicide deaths. Suicidal ideation was found in 43% of bipolar disorder patients. BD is particularly prevalent among creative types.
Neurofeedback provides an effective method of stabilising mood, significantly improving depressive symptoms, and addressing brain areas responsible for suicidal ideation or self-harm. Positive thinking can be restored, as can be sleep, focus, and self-esteem.
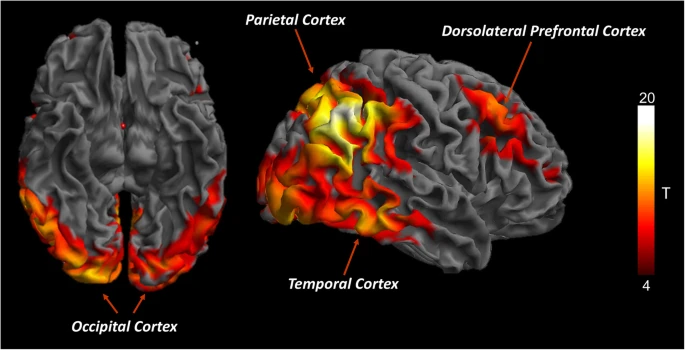
Neural Correlates of Depression
When we look at depression as a combination of issues that can be resolved, we are already on a path of hope and optimism. There are multiple components to this problem, and most start in the mind. We believe it is important to take a holistic view, incorporating physical health (e.g. exercise and nutrition), and becoming realistic about making changes to one’s environment that can turn it from being overbearing to self-supportive.
Within our brain, there are over forty distinct regions that contribute towards our assessment of the world around us and shape the way we interact with others. Humans are made to be social, and constructing healthy, productive interactions contributes towards our own sense of self, creating a feedback loop that furthers our ambitions and emotional fulfilment.
Neurofeedback provides a scientific approach to disaggregating the web of negative thoughts and fears that can put us in a state of depression. The function of different brain areas has been, and continues to be, well-researched, and by putting together these pieces we can get a more granular understanding of our individual sources of depression.
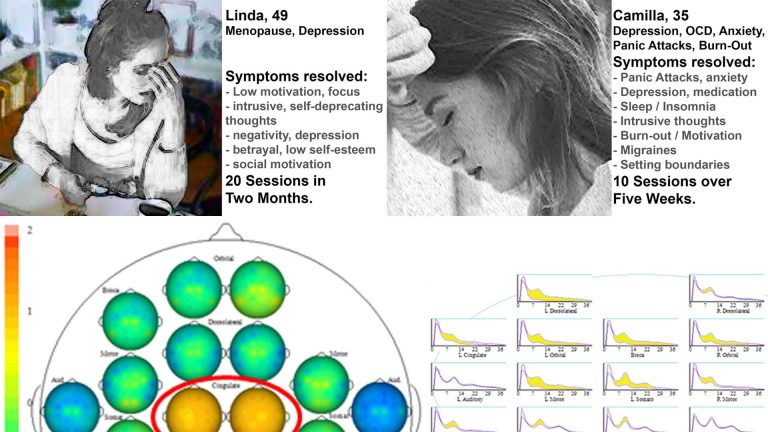
A Kaiser Neuromap shows us which brain areas are dysrhythmic, and with neurofeedback we can train these areas to function optimally. This process equips our mind with the ability to be more constructive in our interactions and general functioning, and thus shape our environment to become self-reinforcing. In general, we notice substantial changes within 10-20 sessions.
Research shows that there are specific brain areas and cortical networks that are responsible for each of the following manifestations of depression. Each person is different, and might only suffer from a few of these becoming dysrhythmic. This is why our training is personalised, based on a Kaiser Neuromap assessment.
– mood regulation and drive
– focus, planning and organisation
– sense of self and feeling part of something, inclusion
– rumination about the past, worry about the future
– anxiety in its various forms, e.g. “what’s next”, social, body awareness, sensory overload
– self-criticism, intrusive thoughts, self-harming tendencies (these can be subtle)
– sleep, both onset and quality (slow-wave sleep and REM)
– the ability to self-soothe, rationally talking oneself down from situations, remaining calm and stable
With Personalised Brain Training we take a holistic approach to restoring the brain’s functionality and aim to restore the concurrent harmony of network interactions. We find that in the process, many issues are resolved and we are able to better synchronise with our environment and again live in the moment.
Medication Reduction accompanied by Neurofeedback
Medication has been a liberally prescribed for depression, used by 15% of the UK population and a quarter of those have been taking them for five years. There are many reports about the trade-off between efficacy and long-term emotional numbing that can adversely affect libido and relationships. Side effects and difficulties in discontinuing their use as well as increased risk of death from cardiovascular disease and all cause are also documented. While effective for some, the “chemical imbalance” model has been debunked, and research into efficacy and specificity provides a spectrum of results, noting that 78% of trials were funded by pharmaceutical companies.
NHS guidelines for their prescription have just been changed to encompass alternatives.
Neurofeedback takes a holistic, personalised approach to mental health, which is non-invasive and medication-free. Moreover, training the brain is a process that helps us reshape our environment to become self-reinforcing in a positive way. It is a complementary therapy rather than a substitute for medical attention.
We have helped many people exit their dependence on medication, and a case study is shown below. This process was, and should be done under supervision of the prescribing entity, and we have found the medical professionals involved to have been supportive. See Case Study Camilla below.
Anna was prone to strong intra-day mood swings as well as having endured a manic episode, during which she became the subject of financial and emotional exploitation. Importantly, Anna was not psychotic; however she suffered from strong attachment disorder, fear of abandonment, some social awkwardness as a result of an impaired sense of self, and lack of ability to rationalise emotions, despite her warm demeanour.
Following a particular slump triggered by betrayal, and being subject to physical violence, she began neurofeedback sessions. Her sleep improved immediately, as did her outlook. Within five sessions, she had become her usual optimistic self again, and began looking for a new vocation. Within weeks, she had a new job that combined two of her passions and talents, and on a solid path to recovery and forgiveness.
Anna’s mood regulation has substantially improved during her ten overall sessions; she feels more grounded and motivated, while enjoying the cause of her work and the new people she is meeting.
Lorna had enjoyed what from the outside appeared to have been a privileged life, having enjoyed private education, a lucrative and indeed fulfilling role in the family business, and accumulated some reserves. She had been medicated for bipolar disorder and ADHD from the age of eight, in what she felt was a suppression of her bubbly personality that didn’t conform to parental expectations of ‘order’ or ‘normal’ behaviour. She had always been social and outgoing, enjoyed boarding school, yet she now felt things had come to a head and that she was not living to be the person she could be. Instead, she believed she had conformed to the wishes of her family and ignored her own needs, emotionally, socially, and fundamentally with regard to her identity. Mood swings, disturbed sleep, lack of focus and self-critical thoughts deprived her of joy in her life. As opposed to deprivation of nurture, Lorna had been domineered by her parents, and not been able to develop her own sense of self-nurture. Her identity and sense of self worth were shattered.
Within five sessions, Lorna’s sleep improved noticeably, as did her energy and motivation. She enjoyed doing long sessions, in particular the film “Now, Voyager” with Bette Davis reminded her of her upbringing and situation. After ten sessions, Lorna began working with a talk therapist to reorganise her life and ambitions – teaching in India was a dream she thought could be realised. Her sense of despair had disappeared, and yielded to a slightly overly self-conscious anxiety, which was the first step past numbness. Lorna’s productivity improved and she began to set herself higher goals, leading to some frustration, yet this substantially contrasted with her previous despondency. A further few sessions helped with the self-blame and internal chatter, and Lorna is on a good trajectory.
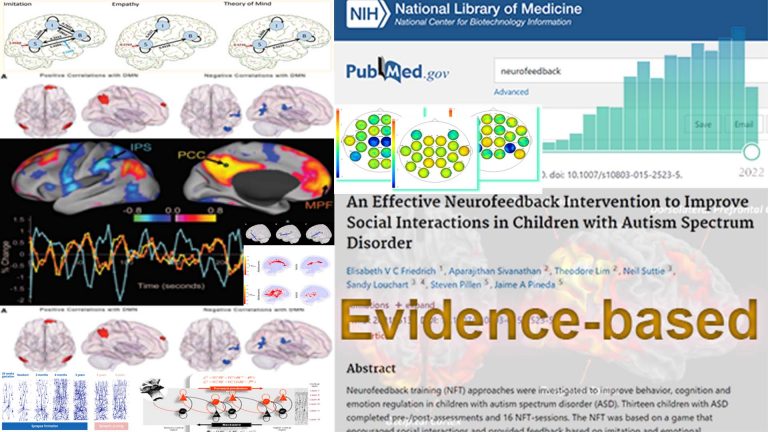
Scientific Evidence: Neurofeedback for Depression
The US National Library of Medicine records over 140 peer-reviewed research papers on neurofeedback and depression, with a significant recent rise in research attention to this non-invasive, drug-free treatment method. Here are some excerpts of the scientific evidence supporting neurofeedback for depression. Note the diversity of brain areas involved, suggesting that depression need not have a single nor consistent source, and the comorbidities often found:
Dr. Corydon Hammond finds in his 2005 paper, “Neurofeedback Treatment of Depression and Anxiety” that neurofeedback training results in “enduring improvements approximately 80% of the time”, with most perceiving a difference after between three and six sessions; a “very significant improvement” after 10-12 sessions, and more so after over 20 sessions.
Twenty sessions of neurofeedback training led to a significant improvement in sleep, anxiety and depression evaluations. The same disorders plus inattention showed significant improvements when conducting ten or more sessions in a naturalistic setting.
Neurofeedback improved depressive symptoms in Major Depressive Disorder (MDD) patients, with significant decrease in anxiety and clinical illness severity noted as a result of the training. Cognitive depression was reduced here. Anhedonia and comorbid anxiety in MDD were also improved in this recent study. Cognitive impairment during MDD is recognised and neurofeedback treatment advocated. Its effectiveness on a variety of cognitive functions in MDD such as working memory, attention and executive functions is established.
Neurofeedback is recognised as a next-generation treatment for Major Depressive Disorder.
Increased happiness ratings, mood improvements and decrease in anxiety was documented with related increased activity in specific brain areas. Cognitive-affective brain areas as neural targets for treating depression are recognised here, while higher-order visual areas are implicated in this study that recognises that neurofeedback training can reduce depressive symptoms by over 40%. Further success in treating MDD with comorbid anxiety symptoms was documented here, training specific brain areas.
Sub-threshold depression was improved in college students and recommended as an effective new way for college students to improve self-regulation of emotion.
Rumination, a maladaptive emotional-regulation strategy, was found to have a neurological basis that was successfully reduced while ameliorating depression. The tendency to preferentially attend to negative stimuli in the world and negative thoughts in mind during depression was found to be controllable with neurofeedback. Ruminative processes and avoidance when dealing with autobiographical memories were attributed to specific brain areas and recognised as contributing to Major Depressive Disorder, promoting neurofeedback training as a depression treatment. Similar brain areas when trained with neurofeedback resulted in improvements in self-esteem.
Training brain areas responsive to negative stimuli decreased negative cognitive biases in MDD, showing greater decrease in self-reported emotional response to negative scenes and self-descriptive adjectives. Neurofeedback training is also able to improve processing of positive stimuli in MDD patients. Another recent study achieved significant improvements in reducing the severity of depression and rumination in MDD training a different brain area. Lasting effects of reinforcement learning of better brain habits on rehabilitating emotion regulation in depression through neurofeedback were found. Depressive symptoms were alleviated consistently.
The treatment resistance of recurrent depression is linked to rigid negative self-representations during an identity formative period in adolescents, with potential lifetime repercussions. The study finds neurological evidence for which it recommends neurofeedback interventions. Significant and lasting improvements following neurofeedback training were discovered in another study on Treatment Resistant Depression (TRD). Significant reduction in depression symptoms were reported after four neurofeedback sessions in patients showing no response to current pharmacological or psychological therapies for depression.
Post-operative depression and anxiety, pain, difficulties sleeping and attention and memory problems were resolved in 20 neurofeedback sessions. The 45-year old female was able to return to work subsequently. Cancer patients found non-invasive, drug-free neurofeedback to ameliorate pain, fatigue, depression and sleep. Chronic Stroke victims found neurofeedback therapy to reduce anxiety and depression level while improving motor, verbal and cognitive skills.
Opiate addicts treated additionally with neurofeedback showed greater improvement in depression and somatic symptoms, and relief from withdrawal, as did cocaine addicted individuals.
Multiple Sclerosis sufferers saw depression, fatigue and anxiety reduced, and the results were maintained at a 2-month follow-up.
Elderly patients found a significant improvement of their depression condition following neurofeedback treatment.
Surgery Residents with burnout and depression saw a return to a more efficient neural network following neurofeedback training.
Neurofeedback has been shown to improve sleep quality and sleep onset as early as 1982, with substantially more research interest confirming this in recent years, also in relation with pain and seizures.
Neurofeedback was shown to additionally benefit patients undergoing Cognitive Behavioural Therapy.
Comorbidities of Depression
Autism is a spectrum disorder characterised by social integration issues and developmental delays that can be both physical and emotional. With a Kaiser Neuromap we can identify individual weaknesses, and train these with Personalised Brain Training in a non-invasive, medication-free manner. Improvements are evidence-based and impressive.
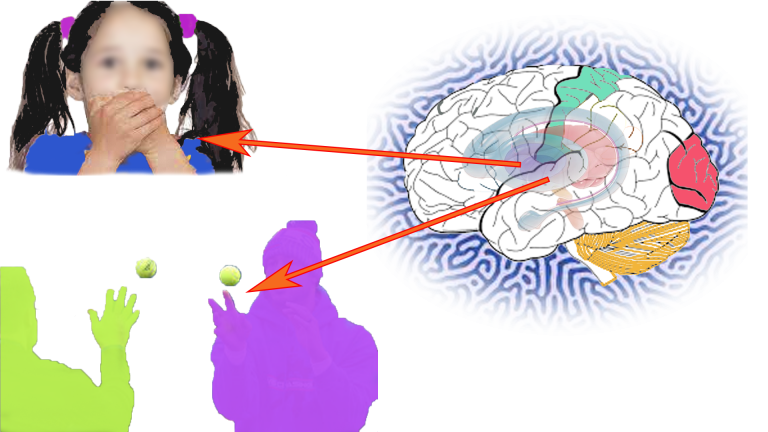
There are distinct brain areas that interpret the respective sensory input, and through various convergent processing stages – multi-modal association areas – the brain constructs a scene, and understands where we are with respect to our environment. When any of these brain areas becomes dysrhythmic, our interpretation becomes distorted, for example, we can become hyper- or hyposensitive, as is seen in various symptoms of autism.
With neurofeedback, we can train the brain areas relevant for efficient sensory processing and integration. Personalised Brain Training uses the most advanced qEEG brain map interpretation method to form an individualised training plan. Our neurofeedback method applies the most effective training protocols with an enjoyable feedback process, watching movies of choice.
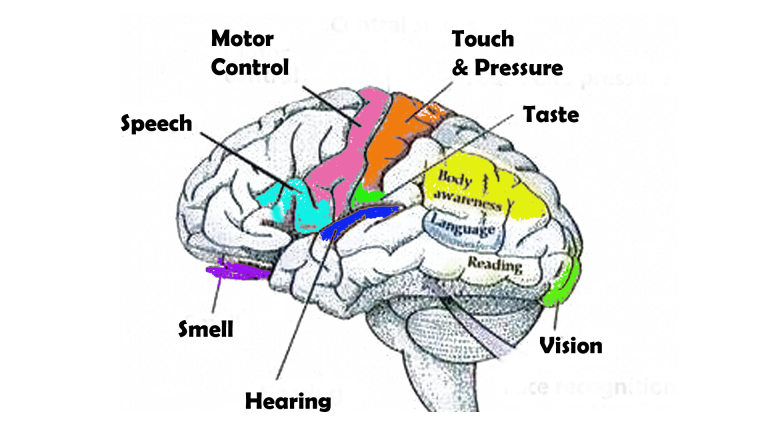
Sensory processing is a well-researched process that involves many dedicated brain areas, and their interaction to produce an impression of our environment, and how it relates to us. Higher integration of ensuing awareness leads us into the realm of “what is consciousness”:
Science shows that our brain is engaged in a constant process of modelling, or predicting, our environment, both with regard to space and time. It does so on the basis of previous sensory information, as well as recent and consolidated memory. Predictions are then matched with reality, and the process begins again. This is an important distinction from the idea that we are merely reacting to our sensory input. It introduces the theory that we essentially anticipate the next moment, and then update our model of our environment, continually.
Autism can be viewed as an impaired capacity to efficiently engage in this predictive process. The theory easily explains the insistence on sameness and inflexibility with regard to changing routines, embracing novelty, interacting with moving objects, reduced appreciation of humour and even Theory of Mind, which is essentially the creation of a model of another person in one’s own mind. An unpredictable world becomes overwhelming, explaining the fear and anxiety we so often witness with the condition, and resorting to self-stimulation (stimming) is an anxiolytic response. As a result of reduced modelling and predictive capacity, repetition is favoured, and this can turn into a strength as replicative behaviours enhance certain skills or narrow areas of focus.
We can think of autism as brain dysregulation in multiple functional areas. This results in many comorbidities, which we implicitly address with neurofeedback training as part of a holistic approach.
Some of the challenges we have seen to improve with neurofeedback training include:
– lack of bodily awareness, motion control and speech, spatial awareness
– an inability to express, understand and convey emotions and physical needs
– increased frustration at not being understood, whether on a basic survival needs level or in more emotional / intellectual areas
– impulsive aggression, potentially morphing into self-fuelling rage and violent behaviour, sometimes self-directed
– perceived lack of empathy and regard for the needs of others
– generally being ‘misunderstood’, to the detriment being able to fully develop strengths and talents
With neurofeedback training, we can address these ultimately self-harming divergences and bring out the incredible potential in all of us.
Neurofeedback training has been shown to be a safe, feasible, and effective therapy approach to Autism Spectrum Disorder across all ages.
Multiple studies confirm:
– improved cognitive flexibility
– improved facial recognition
– better behaviour, including being less aggressive, more cooperative and better at communication
– improved functional connectivity in the social brain regions.
A 9 point improvement in IQ was reported alongside decreased ASD symptoms including attention, anxiety, aprosodias, social functioning, as well as academic and intellectual functioning.
Sensorimotor behaviour (posturography) improved in children.
Neurofeedback training has proven calming effects.
Research evidence for comorbidities, e.g. ADHD, dyslexia, depression, anxiety, seizures, sleep and behaviour is shown under the relevant tabs below.
Our brain controls our movements. Functional connectivity dysregulation in autism can affect many of the brain areas involved in planning and executing motor actions. With neurofeedback, we can train these areas to improve symptoms in an evidence-based manner.
There are various cortical, and sub-cortical brain areas involved in motor coordination. With neurofeedback, we are training the cortex. Many cortical areas have deep connections to the basal ganglia and cerebellum, and it appears that we are training these deeper structures implicitly.
In our experience, the following issues can resolve with neurofeedback training:
– motor issues, such as dyspraxia and lack of coordination
– stutter and speech production
– facial tics
– uncontrolled, compulsive movements and actions.
Before and after brain maps corroborate these findings; research has so far focused on neuromarkers for these phenomena, and suggest neurotherapy as an adjunct to traditional therapies.
Tourette’s Syndrome can involve many of the above issues, as well as lack of executive control, again an aspect we have seen improve substantially with neurofeedback training.
Lack of mood regulation, self awareness, and inhibitory control contribute to anger management and behavioural issues. These complicated behaviour patterns have a neural basis and vary by individual. With a Kaiser Neuromap we can detect vulnerabilities and train these with neurofeedback.
Excessive obstinacy, misunderstanding social cues and general overwhelm and anxiety are frequent characteristics of autistic children. With neurofeedback training, we have had success in remediating these symptoms.
Multiple brain areas contribute to impulsive aggression, self-fuelling rage, physiological arousal, ‘acting out’ and conversely calming down and rationally understanding one’s behaviour and even showing regret, remorse, understanding and insight, or not as the case may be.
A Kaiser Neuromap shows us possible vulnerabilities to such behaviour patterns, and can help us form a more nuanced understanding of a person’s preconscious drivers, that is, their ‘wiring’. There are multiple contributors which we can address:
– impulsive aggression, e.g. in response to being denied something
– rage, a continued unconsolable stage
– lack of empathy or understanding of others’ feelings
– inability to see different perspectives
– turn taking, self/other differentiation, shared authority
– monitoring and understanding consequences of actions
With neurofeedback training we can work on these preconscious processes, which occur before a person is able to apply conscious control or inhibition. The aim is to reduce or eliminate the person’s propensity to exhibit such adverse and undesirable behaviour in the first place, freeing up the mind to enjoy the moment in constructive synchrony with others.
Neurofeedback helps us stabilise the Default Mode Network, and reduce impulsive aggression and physiological arousal control. We have seen success within a few sessions in clients from 8-15 years of age.
Impulsive aggression can become self-directed at times. This irrational urge is often triggered when an autistic child doesn’t get what they want, or feels misunderstood and frustrated. Self harm can also take the form of resignation, accepting less than one’s worth, and thus denying oneself recognition and opportunity.
Neurofeedback calms the mind and we can address brain areas contributing to self-harming ideation and intrusive thoughts.
We look to improve sense of self, reduce anxieties and strengthen inhibition levels while reducing self-directed impulsive aggression.
‘Self-harm’ can take many forms, and beyond physical manifestations (e.g. cutting, suicidal thought or even action) it can be more subtle:
– Accepting less than what we’re worth, overly and unnecessarily acquiescing to the perceived demands of others when not at all in our own self-interest, self-deprecation
– an inability to defend one’s own stance and needs are often overlooked and can be very harmful to a person’s development, especially when repeated and consolidated into a character trait.
With a Kaiser Neuromap we can detect vulnerability to such behaviour, including suicidal tendencies or ideation.
This is not diagnosis and it is non-specific in that dysrhythmia of the brain area(s) responsible for this is a necessary, but not sufficient condition. Nevertheless, it is a worthwhile finding that can help prevent worse outcomes by prompting awareness and intervention.
With neurofeedback training, we have helped self-harming adolescents transition from ‘cutting’ and dissociation to becoming engaged young individuals who are able to stand their ground, maturely deal with setbacks and embrace the sense of being part of a community.
Neurofeedback is a complementary therapy and medical attention should be sought in cases of self-harm.
There are many manifestations of anxiety, including social anxiety, panic attacks, excess body awareness (body dysmorphia), emotional hypersensitivity, fears and phobias. Autistic children generally present with a variety of these, all contributing towards an energy-consuming heightened state of vigilance. Stress and defensive behaviour results.
Neurofeedback is an established, evidence-based treatment for anxiety.
It was found that neurofeedback training for anxiety and depression “results in enduring improvements approximately 80% of the time”
Confidence and social integration tend to improve accordingly, resulting in a positive feedback loop that helps shape new trajectories.
A brain map will reveal overactivity of brain areas responsible for monitoring consequences of actions (timidity, general fright and reticence); watching out for an abuser (bully); body and face awareness; and excessive self-monitoring. This helps us understand the potential presence of real threats and fear factors. We can also detect possible tendencies to develop unhealthy body awareness. Neurofeedback training lets us address this issues.

There are multiple types of anxiety, each correlating with one or more brain areas being dysrhythmic:
Social anxiety: When we’re in a situation with other people and our understanding of the social dynamics and complexities is overwhelmed.
Sensory overload: our brain interprets all sensory stimulus as directed to ourselves. We lose the ability to discern what is directed at us, and which matters or interactions are of no concern to us. This sets us up for panic attacks and ultimately psychosis. It also means we become singular in our perspective, unable to take on other points of view
Loss of narrative: Our episodic understanding of the situation, how we got there and what happens next, is impaired, and we are unsure of where we are and where we’re going. This hyperactivates our amygdala, and the sensation is highly emotional
Auditory sensitivity: we become prone to overly interpreting the emotional content of words and sounds, creating an air of prickliness and pushing people away without knowing it
Activation: Our ARAS is responsible for setting the right level of physiological arousal, or wakefulness, for the situation, and to remain stable there. When this is on overdrive, we are pushed further into fight-or-flight mode than necessary, thus heightening sensory sensitivity. Panic attacks are an extreme manifestation. Our ability to calm down quickly is reduced.
Trauma: an inability to self-nurture – creating an emotional safe-space around us – and self-soothe – being able to talk ourselves down rationally from a situation, thus resulting in mood instability. This can also manifest in dissociation and heightened pain perception. We ruminate about the past and worry about the future, instead of being able to enjoy the present.
Intrusive thoughts: Self-criticism overshadows motivation and confidence, and we become self-aware and distracted by negative thoughts and feelings. Some use acquired habits to distract from this. Others become attached to the reward circuitry triggered, and sustained by feeding obstructive, self-deprecating thought content. Our confidence, motivation and social interaction suffer as a result.
The vernacular description of ADHD has come to include many other issues than its core definition of distractibility and/or hyperactivity. We often find many other comorbidities, such as behaviour problems, impulsive aggression, rage, excessive stubbornness, various anxieties, mood dysregulation, sleep problems, dyslexia and inappropriate social skills.
With a brain map, we can assess vulnerability to a host of other possible issues, and then address these with neurofeedback training in a personalised manner. Furthermore, we have a chance at promoting structural improvements, such as prefrontal brain maturity. The core issue of ADHD, Distractibility, is dealt with here:
Focus and Productivity have three core components:
– Concentration
– Planning and Organisation
– Motivation
Each of these three components is governed by a different brain area. When one or more of these regions is dysrhythmic, we are vulnerable to focus issues.
– Planning and Organisation: understanding goals, working back to the present and structuring a workflow conducive to achievement, seeing the bigger picture and dividing projects into tasks, prioritising these and being flexible.
The ability to form an overview of the task at hand, break this down into smaller, manageable steps, and sequence these accordingly, can be trained.
– Concentration: the ability not to be distracted and maintain attention on the relevant task at hand. Distractibility is a function of spatial awareness, and there are brain areas dedicated to this task. When they are dysrythmic, we become easily distracted.
– Motivation: having sufficient drive, optimism, persistence and endurance to implement plans and overcome setbacks. Self-esteem, an understanding of one’s own strengths and weaknesses, and the ability to self-soothe, that is, to rationalise thoughts, are key to this.
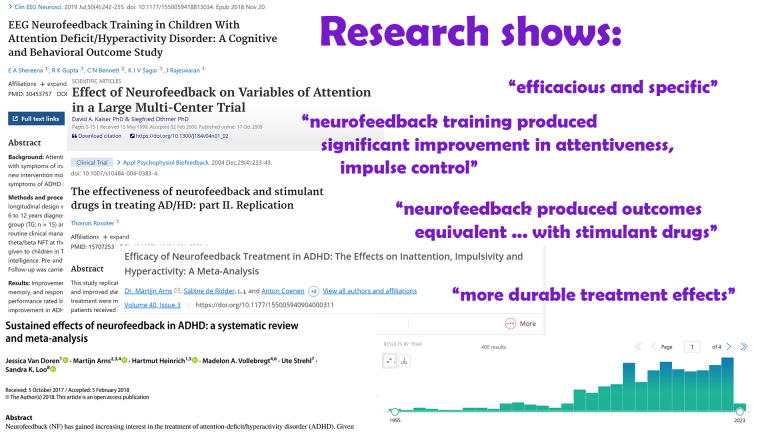
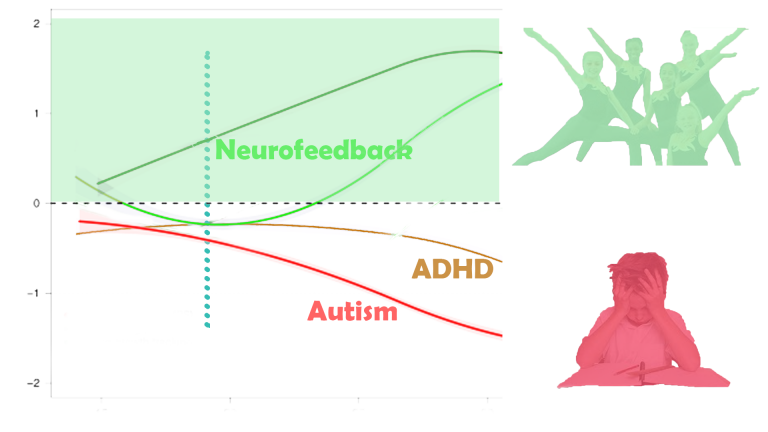
Researchers conclude that neurofeedback training can be considered “Efficaceous and Specific” (Level 5) for ADD / ADHD. Neurofeedback training was shown to produce significant improvement in attentiveness and impulse control. It was shown to produce outcomes equivalent to those obtained with stimulant drugs. The effects were shown to be long lasting.
Neurofeedback and ADHD Medication
We have successfully helped children and teenagers reduce or discontinue stimulant medication treatment of ADHD where this has become undesirable, under supervision of the prescribing entity.
Individuals may offer motivations to change stimulant medication use to alternate forms of therapy, including ambiguity concerning long-term use and reduction of symptom-severity effectiveness at the cost of growth (height). Many are considered “prohibited substance” in competitive sports, being listed as Schedule II / Class B substances when obtained without prescription. Possible sleep problems are documented.
There appears to be a range of conclusions in studies regarding the effect of psychostimulants used to treat ADHD on mood, anxiety, emotional reactivity, substance abuse, psychiatric conditions, cardiovascular implications, tics and other dyskenisias, among other, and these vary considerably in sample size, duration and scope.
A study with over 130 participants showed that neurofeedback can be used effectively in combination with pharmacological treatment, enhancing results.
See here for more information.
Research on Neurofeedback and ADHD
Neurofeedback training for ADHD is evidence based and produces lasting results:
Attention deficit: Efficacy is well-documented – there are over 370 research reports on Neurofeedback and ADHD on PubMed.
In line with AAPB and ISNR guidelines for rating clinical efficacy, neurofeedback can be considered “Efficacious and Specific”, the highest level (5), with a large effect size for inattention and impulsivity in this study.
A large-scale study showed that neurofeedback is effective in remediating attentional dysfunction. Significant clinical improvement in one or more of attentiveness, impulse control, and response variability was observed in 85% of participants after 20-40 training sessions.
Impulse control and attention improved through neurofeedback training, producing “patient outcomes equivalent to those obtained with stimulant drugs”
Neurofeedback “appears to have more durable treatment effects, for at least 6 months following treatment.”
Neurofeedback was shown to be an effective method to enhance cognitive deficits, reduce ADHD symptoms and behaviour problems in children. The effect was maintained in a follow-up six months later.
There are numerous academic studies confirming the efficacy of EEG biofeedback (another name for neurofeedback) with sustained performance gains.
The American Academy of Pediatrics bases its conclusion that there are “no significant contraindications” to its use on these studies.
ILF / Othmer Method neurofeedback training was shown to reduce ADHD symptoms, specifically distractibility and impulsiveness, in a study involving 251 children over a course of 30 neurofeedback sessions.
Training specific brain areassuccessfully activated error monitoring networks in ADHD patients, associated with symptom improvements. Dynamic functional connectivity was found to be maintained in a follow-up 11 months later.
Another study attested improved response control and attention in ADHD post Neurofeedback.
Mood regulation and Motivation: see here
Working Memory: see here
Sense of Self: With Personalised Brain Training, we work on the Default Mode Network, the neural basis of self.
Dyslexia often presents together with ADD/ADHD and other behavioural issues. With a Kaiser Neuromap, we can assess vulnerabilities, and then train these with Personalised Brain Training.
Dyslexia is an impaired ability to understand written and printed words or phrases and affects 10-20% of the population in both males and females. The disorder can result in learning difficulties, poor academic performance, stigmatisation and ensuing behavioural issues.
While often classed as a disability, there are associated strengths: creativity, the ability to solve complex problems, unorthodox approaches to ideas and projects, and a more detached ability to apply logical thinking are some of these. Nonetheless, the condition can impair school and social functioning, slow maturation and significantly affect self-confidence and -esteem.
“Picked up a book and started reading! Unheard of before, I could never get her interested in reading for herself.” – Mother of Anna (9)
There are neural correlates with dyslexia which we can train with neurofeedback.
Reading and comprehension involves multiple brain areas as well as their seamless communication. We have Wernicke’s area for comprehension, and Broca’s for speech generation. Additionally, there are regions involved in sequencing, visual recognition, focus and attention, and contextualisation or syntax recognition of subject matter along with various memory-related areas.
It is important to note that there are different types of dyslexia. A brain map shows us which brain areas are dysrhythmic.
With neurofeedback, we train brain areas involved in visual and auditory processing; memory; focus and attention; syntax and context; sequencing and organisation. We also train the connections between these areas. The approach is holistic: we work on core networks, and their integration with each other.
Research on Neurofeedback and Dyslexia
Research has shown that neurofeedback training can improve reading ability and phonolocigal awareness deficit in children with reading disabilities, as well as improvements in spelling.
For a summary of 18 neuroscientific research studies on language learning impairment produced until 2015, see here.
One in four persons with ASD are non-verbal, and 40% of all children referred to an autism clinic have significant speech delay, regardless of diagnosis.
Infants begin to understand and produce single words and gestures in the context of playful interaction from 12 months of age; between 18-24 months there is a rapid expansion in vocabulary and knowledge of rules regarding conversational exchange. Typically developing children will use language for social interaction; this contrasts with ASD children who are more likely to use words to regulate their environment (demands, protest), rather than with communicative intent. Despite the range of language abilities, articulation skills are generally spared. There is a strong link between language and social skills in autism.
Speech development has numerous components, all of which have neural correlates, meaning there are brain areas contributing towards language comprehension and generation, which have to mature and work together efficiently. This means we have a chance to improve speech generation by training the brain, and both research and experience confirm this. The research below illustrates how we can assist with improving necessary building blocks that contribute to a person’s development of speech and language capabilities.
Speech and language development are also a function of social reciprocity, both with regard to initiation and reception. It should therefore not be seen in isolation, and rather as an accompanying component of improving effective synchrony with the social environment.
Personalised Brain Training takes a holistic approach to improving social integration by way of training various features of cognition and consciousness, including sense of self, joint attention, Theory of Mind, focus, mood regulation, behavioural challenges and communication, both verbal and non-verbal.
Research on Neurofeedback and Speech
Neurofeedback training was shown to improve speech-in-noise perception and auditory discrimination that was applicable post training and long-lasting. This shows that we can positively affect neural encoding of acoustic inputs in the auditory cortex, a frequent issue with autistic individuals.
In ADHD children, neurofeedback training improved visual memory, enhanced auditory short-term memory and auditory working memory.
Biofeedback produced better and more lasting effects than traditional therapy in behavioural dysphonia.
Neurofeedback was shown to improve the ability to identify emotional prosodic intonations.
Phonetic recognition and reading skills have been shown to improve with neurofeedback training, another important component of speech and language acquisition (see “Dyslexia”).
Personalised Brain Training is a holistic approach; we also train brain areas relating to focus, motivation and sense of self, as well as sequencing and motor skills, all of which contribute to the development of speech.
Sleep is where we recover – physically, mentally, emotionally.
It is a complex process whereby the brain enters different behaviour patterns in various stages. Slow wave sleep is where our body recovers; REM sleep is where we digest the day’s experiences, consolidate what we’ve learned and let our brain process memories and impressions.
Ideally, we would like to be able to switch off once comfortable, enter a deep sleep and wake up restored and energetic. If our sleep suffers, so do our concentration, productivity, physical abilities and emotional flexibility.
Neurofeedback has been shown to improve sleep quality and sleep onset as early as 1982, with substantially more research interest confirming this in recent years, also in relation with pain and seizures.

"I felt so calm last night! And slept like there were magnets between me and the bed. 10 hours straight."
"Slept like a log."
"Since I started neurofeedback training, my dreams have come back!"
Client testimony.
One of the first discoveries made in the exploration of EEG, fifty years ago in 1972, was the ability to improve seizure resistance through neurofeedback.
An analysis of studies indicated that 82% of subjects demonstrated significant (more than 30%) seizure reduction, with an average value of 50%.
A 2009 review of studies established that EEG operant conditioning was found to produce a significant reduction on seizure frequency.
Barry Sterman was able to cure a 23-year old female epileptic from seizures using his SMR-biofeedback training over the course of two-and-a-half years.
Another pioneer of the field, Joel Lubar, reached similar results.
In our experience, neurofeedback has improved seizure resistant in many cases, and has always been beneficial in the treatment of secondary mental health effects. Medical attention should always be sought, and sources can be diverse and elusive.
Traumatic Brain Injury (TBI) is another application of neurofeedback training.
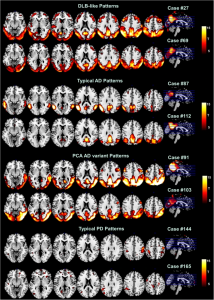
We have found neurofeedback to be highly effective in assisting physical rehabilitation. With a Kaiser Neuromap, we can detect areas of hypometabolism that respond hemodynamically with neurofeedback training. There are neuromarkers for mTBI, as well as Alzheimer’s Disease, though these are non-specific (necessary, not sufficient conditions) and should not be seen as diagnosis. General (rather than focal) lesions in neurodegenerative conditions appear to form first in the corpus callosum, a fibre bundle linking the two brain hemispheres; altered functional connectivity has been visible there on a brain map too, in our experience, at an early stage.
There is evidence that neurofeedback supports myelination, improving the important sheathing of axons, which is a critical part of the physical recovery process.
Pain perception has neural correlates – there are brain areas that govern our attentiveness to the signs our bodies are giving us.
In the first instance, these signs are real messages that something is wrong and needs dealing with. Medical attention should provide solutions to this.
Sometimes, pain perception can become irrational in this context, and with neurofeedback training we can help the brain establish a more reasonable approach to interpreting such stimulus.
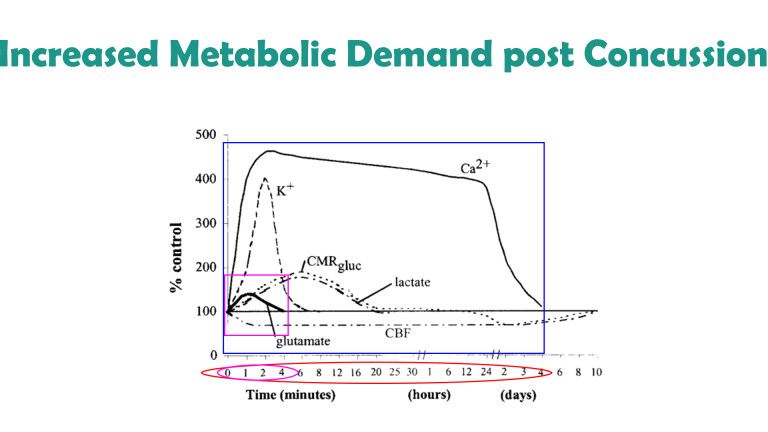
Immediately following concussion / mTBI, there is an increased demand on energy (glutamate) in the brain, at the same time as cerebral blood flow is constrained.
This effect is most pronounced during the first four minutes following impact; other neuromodulatory impairments last for days, and it is estimated that cerebral blood flow is only normalised after around ten days. The blood brain barrier is temporarily disrupted in the first few minutes leading to a complex inflammatory response in the hours and days following injury, and microglia can remain activated for many years.
There are numerous neuromarkers of mTBI, ranging from reduced prefrontal activation to impaired Default Mode Network functionality; while these are non-specific – necessary, but not sufficient conditions – some are highly unusual and show up on a Kaiser Neuromap. With neurofeedback, we can train these, while restoring general functionality of our neural basis of self (the Default Mode Network). We have seen impressive recoveries, both with regard to client feedback and before/after brain maps.
Concussion / mTBI increased the risk of Alzheimer’s Disease by 50% and shares similar mechanisms of promoting tau / amyloid pathology. TBI also increases the risk of Parkinson’s Disease and is capable of producing a prion-like spread of self-seeding proteinopathy. Moderate to severe TBI adds around five years to measured brain age, relative to chronological age.
Schizophrenia
Schizophrenia comprises a wide range of thought disorders, which ultimately affect an individual’s ability to share a reality with others. Causes can be trauma, emotional or physical; drug use; stress; genetics.
With neurofeedback training we aim to restore a healthy sense of self; flexibilise the social brain; and ameliorate comorbidities such as intrusive thoughts, mood disorders, focus and attention issues, paranoia and anxieties; and psychosis.
Neurofeedback training can improve functional connectivity and strengthen white matter tracts, both of which are impaired in Schizophrenia.
Each person is different: with a Kaiser Neuromap we assess individual vulnerabilities and train these with neurofeedback. Personalised Brain Training enables the person to unfold their genius in a socially reciprocal manner.
Neurofeedback is medication-free, non-invasive and evidence-based.
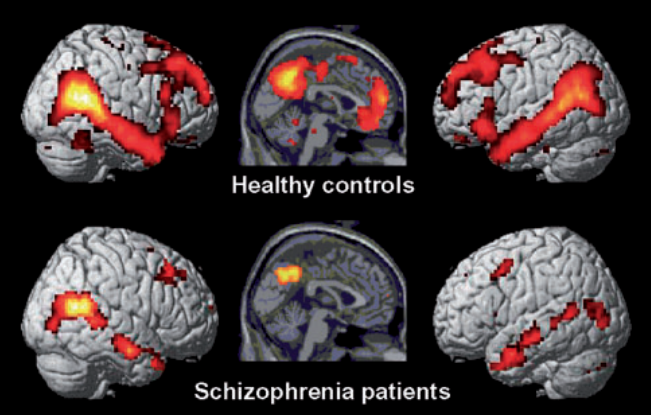
While there are certain commonalities between sufferers of schizophrenia, no two brains are the same. On the basis of a brain map we can identify particular vulnerabilities and work on these specifically.
Neurofeedback training can help restore the integrity of the Default Mode Network, the neural basis for ‘self’, as well as switching between self-referential states and active modes (the Central Executive and the Salience Networks).
Emotional self-regulation can be improved and anxiety, depression, sleep and focus issues alleviated.
Neurofeedback can calm the brain and help manage the ‘Voices’, as well as other regions prone to over-priming external agency. Significant reduction in Auditory Verbal Hallucinations (AVH) has been achieved with neurofeedback training.
Psychosis is a state that can occur, and recur, in persons diagnosed with Schizophrenia, Bipolar Disorder, Trauma and neurodegenerative conditions. Note however that it is not a necessary condition for any of these.
Daniel Webster of Neurofeedback London-Brighton has extensive experience working with Schizophrenia patients. Research and experience have shown effectiveness of neurofeedback training for Schizophrenia and its various comorbidities (see other tabs)
Trauma, (C-)PTSD
Trauma and abuse leave scars.
When the viability of our existence has been subjected to threat, our behaviour adapts. We become primed for hypervigilance, sensitive to triggers, and our physiology responds accordingly. A heightened sense of awareness now confers safety, and we can even become addicted to this.
Our brain keeps the score: Areas responsible for defence and vigilance are activated, even when there is no objective reason. Sensory stimulus is amplified, and we dedicate value energy resources to the monitoring of others’ intentions. Anxieties are rekindled, and the strain on our system leaves us exhausted while unable to switch off and effectively recuperate. Our focus and productivity drop, as does our self-esteem. We can feel detached from our bodies, dissociating. Our social capacity is impaired.
Neurofeedback helps us break this cycle: we equip the brain to get over it, to get on with it, re-establish our sense of self-worth, and the ability to constructively engage with our environment. We gain a healthy sense of detachment, which allows us to process the past more efficiently and look forward to the future.
With a brain map, we can identify which parts of our system are being particularly stressed. Neurofeedback training helps us bring these brain areas into better alignment.
Typical Symptoms of Trauma and PTSD
The first indication that we are experiencing trauma / PTSD is when we find ourselves not living in the present. Enjoyment of the moment and social interaction is clouded by constant ruminations about the past, and worries about the future. We are unable to ‘let go’, relax, and grasp opportunities as they present themselves in the Now.
We are plagued by intrusive thoughts that bring us back to events in the past, which needn’t even be related to a traumatic event, but which remind us of some inadequacy and amplify our self-doubt. Feelings of shame and guilt come into the picture as well, further eroding our self-confidence. “How can I be happy and enjoy this after what has happened?”. Similarly, our perception of the future is shrouded in worry and fearful anticipation. Uncertainty is our greatest foe, our perception of safety is unhinged by any doubt as to what could happen next.
The absence of a plan becomes a concern, the lack of clarity as to what’s around the corner a burden. Negativity associated with the past deprives us of hope. We are thus unable to see uncharted territories ahead as an opportunity, and much rather dwell on impending threats.
Indeed, our system is primed to protect us, and we are in survival mode. This process becomes self-feeding as we become addicted to the hyper-arousal our sense of fear induces. Our sense of joy and looking forward to fun becomes clouded to the extent we forget and no longer yearn it. Detachment sets in, further isolating us from feelings that previously motivated us. This process can even start slow and subtly, yet the cycle is self-fulfilling and deprives us of the necessary perspective to break and get out.
In Personalised Brain Training, our definition of trauma is wider. We include for example perceived loss of social standing, which can be either the cause or the consequence of a traumatic event or development. The perceived loss of social position results in us feeling judged. We become hypersensitive to how people approach us, talk to us, deal with us.
This is a subjective concept, as it should be, given that trauma should be recognised as an issue of perception by the affected person, rather than a concept being ‘awarded’ by an unrelated party, though external affirmation can help and medical advice should be sought in any event. As humans, social recognition is a critical component of our biological drive to propagate. Attraction relies on this, which ultimately leads to bonding.
Consequently, there are numerous brain areas devoted to, or involved in, the assessment of our position with regard to others. When our self-perception is assailed, or even the viability of our self is questioned, we are naturally shaken. Various brain areas become dysrhythmic. These include areas responsible for our body control and awareness, and many therapies focus on engaging the body and somatosensory system with a view to inducing cerebral changes.
However, this is only a part of the picture – there are many, arguably more powerful neuronal centres in the brain that are affected by trauma, and with a Kaiser Neuromap and Default Network Training (together, Personalised Brain Training), we can assess the issues more accurately, completely and efficiently, as well as then successfully training the brain to overcome trauma and setting ourselves on course for a positive trajectory.
Another consequence of trauma is that we may feel unable to rationally assert a sense of safety. This is different to self-nurture, or an emotional sense of safety. When we are unable to talk ourselves down from a situation we lose the ability to effectively regulate our moods, to switch off when we need to, and ultimately can become excessively paranoid.
There are neural correlates for this behaviour, and we can asses this with a Kaiser Neuromap. Safety and assurance are core needs we are programmed to seek to fulfil. Authority and role models help us in this quest. When we become dysregulated in our ability to self-soothe, we are also compromised in our ability to find paternal guidance. As a result, we tend to over-idolise figures who seemingly exude strength and power, or disobey completely and become unnecessarily rebellious – both immature behaviour patterns. Resetting this balance is crucial to achieving calming, regulated emotions, reduced hypervigilance and controlling impulsiveness. Personalised Brain Training lets us achieve this.
When hypervigilance persists untreated, we face further problems.
Physically, our heart beats faster and harder, more of the time, which is a clear stress on our system.
Mentally, we become prone to developing intrusive thoughts, even when we are able to relax, and more so when we are stressed, where these can take on third-person character, a voice in our head. This can have a destabilising effect, not least because we are now spending energy ‘defeating’ other perspectives we are internally engaged with, and thus distracting us from the ‘now’. Being on hyper-alert can also make us more susceptible to feeling relational to sensory input, in that we feel that everything is directed at us, which can set us up for psychosis.
As we lose our ability to enjoy the moment, our social interactions suffer. Exercising our social brain keeps us alive and forms the basis for sound mental health. Our brains are adaptive, and we need to provide stimulus to maintain connections and sustain flexibility. Isolation deprives us of many necessary exercises. For example, brain areas that deal with face recognition also respond to affective interactions and the ability to discriminate between emotional content of faces. We need to keep training these brain areas through social interaction in order to maintain emotional recognition – it is not a surprise that perpetual mask-wearing heightens our social anxiety (aside from adverse physical effects).
Social recognition, a key component of our biological need to attract and bond, is driven by sensory interpretations. Again, we need to exercise brain areas that contribute to this, including language and speech generation and comprehension, auditory sensitivity, and monitoring rewards for actions, both directly and vicariously. Our mirror neuron system contributes towards learning from others’ mistakes or examples, and consequently the storage of social rules necessary for constructive functioning in a society.
Inclusion is imperative to establishing a healthy self-image or sense of self. This in turn is crucial to forming stable relationships with friends, family and forming healthy alliances necessary for personal and professional progression. When we lose our sense of belonging to a group or cause, we may become unstable in our self-perception and our relationships with others. The effect may snowball into perceptions of abandonment, feelings of emptiness and dissociation; this in turn correlates with mood dysregulation, impulsive and often dangerous behaviours, intrusive thoughts and potential self-harm.
With Personalised Brain Training, we can assess vulnerability to these traits as they manifest in functional brain area dysrhythmia that shows in a Kaiser Neuromap; with Default Network Training, an advanced form of neurofeedback, we can train these brain areas and networks in a holistic manner to help re-establish balance. This enables us to reconnect with our environment and re-enter a positive feedback loop.
Sleep is adversely affected by trauma. First, the mind needs to ‘let go’ in order to enter deeper sleep cycles, which is a challenge for many. Excessive rumination and intrusive thoughts can hinder this, as does the loss of our ability to rationally calm ourselves down. The depth of our sleep is governed by our ability to self-nurture and create an emotional ‘safe space’. Homeostasis during various sleep stages is governed by other parts of our brain, some still involving the cortex. With a Kaiser Neuromap we can detect dysrhythmia in the relevant brain areas and train these accordingly with Default Network Training (together, Personalised Brain Training).
Focus and organisation suffers as a consequence of sleep issues. This time, different brain areas are affected, which we can also train. When we are unable to concentrate and produce our best output, we become demotivated and our mood and sense of self suffer. Again, there are brain areas responsible for these aspects of being, for which we can again detect dysrhythmia and provide neurofeedback training. The process is holistic – many components have to work together effectively for us to function optimally.
Mood regulation suffers when we lose social integration, sleep and focus. Neurofeedback training found to significantly help 80% of people with depression by aiming to restore motivation, improving sleep and focus, and reducing anxiety.
There are numerous potential cortical contributors to depression, and with a brain map we can see vulnerabilities.
Neurofeedback training lets us address these as well as establish a generally improved sense of well-being in a holistic manner. he positive effects of neurofeedback training have been shown to be lasting. Neurofeedback is non-invasive and medication-free.
There are multiple types of anxiety, each correlating with one or more brain areas being dysrhythmic:
- Social anxiety: When we’re in a situation with other people and our understanding of the social dynamics and complexities is overwhelmed.
- Sensory overload: our brain interprets all sensory stimulus as directed to ourselves. We lose the ability to discern what is directed at us, and which matters or interactions are of no concern to us. This sets us up for panic attacks and ultimately psychosis. It also means we become singular in our perspective, unable to take on other points of view
- Loss of narrative: Our episodic understanding of the situation, how we got there and what happens next, is impaired, and we are unsure of where we are and where we’re going. This hyperactivates our amygdala, and the sensation is highly emotional
- Auditory sensitivity: we become prone to overly interpreting the emotional content of words and sounds, creating an air of prickliness and pushing people away without knowing it
- Activation: Our ARAS is responsible for setting the right level of physiological arousal, or wakefulness, for the situation, and to remain stable there. When this is on overdrive, we are pushed further into fight-or-flight mode than necessary, thus heightening sensory sensitivity. Panic attacks are an extreme manifestation.
- Trauma: an inability to self-nurture – creating an emotional safe-space around us – and self-soothe – being able to talk ourselves down rationally from a situation, thus resulting in mood instability. This can also manifest in dissociation and heightened pain perception. We ruminate about the past and worry about the future, instead of being able to enjoy the present.
- Intrusive thoughts: Self-criticism overshadows motivation and confidence, and we become self-aware and distracted by negative thoughts and feelings. Some use acquired habits to distract from this. Our confidence, motivation and social interaction suffer as a result.
The primary issue of trauma affects brain areas that are activated during empathy and forgiveness. With these two qualities impaired, our emotional life suffers, as do our social capacities. With neurofeedback training, we can restore functionality of these brain areas. Another reason this is important is because we do not want to become oppressors ourselves. As we lose our sense of emotional investment in our surroundings, we become careless with regard to others’ feelings and needs.
Implicitly, we are now capable of unintended yet real behaviour patterns that can harm others, as we become deaf to feedback. Not only has trauma affected us, it now makes us perpetrators that pass it on.
Besides reduced social interaction and a less meaningful emotional life that is now more self-centred – and with the wrong type of therapy, becomes self-indulgent and self-perpetuating – we can experience a physical withdrawal from our environment. Dissociation can be momentary and intense, or subtle and ongoing to the extent that we are not even cognisant of it. Either way, our bodies retreat from sensations, analogous to our emotional withdrawal.
Many therapies aim to revive our sense of ownership of our bodies, and thus ultimately our life and future, by training our body awareness in various ways. Realising that our bodies are steered by our mind, specifically our cortex, we can train the relevant brain areas that govern our body perception and movement execution.
Neurofeedback training effectively complements these approaches by directly treating the areas involved in perception and interaction with our surroundings.
One of the first manifestations of trauma is in our bodies. Aside from heightened physiological arousal, a form of paralysis can override our natural motions and postures. Stress, and pain ensue, which can often be felt all around the body. Fibromyalgia is a variant of this phenomenon, as are headaches, chest pains, and chronic fatigue.
There are many techniques for combating this form of physical dissociation. Neurofeedback complements these by training the brain areas that instruct the body to behave in this undesirable way. It is a holistic approach, and we restore overall calming while providing the brain with rational and emotional capacity to overcome its challenges.
Menopause can have adverse cognitive and mental health symptoms.
Neurofeedback training has been shown to be an effective, non-invasive, medication-free treatment for many of these.
It is a complementary therapy and evidence presented is based on general applicability, rather than being menopause-specific.
The menopausal transition is often accompanied by mood, memory and sleep issues.
Managing symptoms becomes important to avoid cumulative effects resulting in cognitive impairments.
Symptoms experienced during menopause include:
– weight gain and body awareness issues
– anxiety
– depression
– sexual dysfunction and impaired sense of self
– sleep disturbance
– brain fog: attention and working memory issues
– vasomotor irregularities: hot flashes, night sweats
Personalised Brain Training aims to restore a healthy sense of self by working on brain areas that are core to our individuality, and addressing areas contributing towards anxiety, mood regulation, sleep, memory and physiological self-regulation.
The process is enjoyable – while watching a movie, we obtain a real-time measurement of a particular brain area’s performance. Feedback is given via small changes in volume, which our preconscious mind understands and uses to adjust it’s behaviour, thus learning to be more efficient. The result is a feeling of calm and self-assurance, with improvements in focus, motivation and sleep. Responsiveness can usually be assessed within a few sessions.
Postural Tachycardia Syndrome (PoTS) was first described in the 1940s, refined in 1993 and finally received a specific diagnostic code in October 2022. It is characterised by exercise intolerance and near syncope upon standing upright, elevated pulse (tachycardia) by 30-40bpm within 10 minutes of standing up, fatigue, anxiety and light-headedness. Often misdiagnosed as chronic anxiety or panic disorder, the group of symptoms comprised by PoTS has a biomarker and increasingly considered an autoimmune disorder, rather than only autonomic nervous system dysfunction. Specifically, increased levels of cytokines and chemokines characteristic of an innate immune condition were found, similar to autoimmune diseases like multiple sclerosis, psoriasis, type-1 diabetes, rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
The condition affects females five times more frequently than males, mainly between 15-25 years of age, with over one million affected in the US alone. PoTS symptoms can persist for years, though half of patients find that orthostatic symptoms and functional impairment subside within five years, and of thost most within 1-2 years. It is estimated that 2-14% of Covid sufferers go on to develop PoTS, while 30% of long Covid patients, especially women, meet the diagnostic criteria.
A client presenting with PoTS like symptoms, recovered within three months of starting neurofeedback training, to the extent that the tachycardia was fully under control and anxieties had subsided substantially. Clinical studies will have to prove correlation. Notably, physical symptoms became manageable, from being previously incapacitating, in a relatively short period of time. This result is encouraging, especially with regard to the speed and extent of recovery, and neurofeedback has been shown to be effective for anxiety. Also, in this person, other neurological issues could be detected with qEEG.
Alzheimer Disease (AD) is the most common neurodegenerative disorder. Similar to Parkinson’s Disease, secondary symptoms are neuropsychiatric in nature and can be addressed with neurofeedback training, helping the person to maintain their sense of self, mood regulation and sleep, and contain arising anxieties.
There are biomarkers that allow us to differentiate between Dementia with Lewy Bodies (DLB), Parkinson’s Disease, and Alzheimer Disease. A Kaiser Neuromap gives us a non-specific indication of each, that can assist early onset diagnosis and thus shape the treatment plan at an early stage.
As with other neurodegenerative disorders, physical changes in the brain affect our sensory interpretation of our surroundings, giving rise to neuropsychiatric disorders. We can become relational in our thinking, and specifically with regard to brain areas that are responsible for our interpretation of personal space and social boundaries.
Neurofeedback Personalised Brain Training aims precisely at encouraging cortical participation and help us share a reality with others, counteracting progression of major secondary, and possibly primary symptoms. Rather than promoting a ‘cure’, we are helping affected persons improve their quality of life in many ways.
The link between Alzheimer’s Disease and Herpes simplex virus type 1 (HSV1) has long been established, as summarised in this research paper from 2014. Four out of five people carry the herpes virus, with one in four being prone to physical symptoms upon periodic reactivation, e.g. blisters / cold sores occurring during times of stress and/or immunosuppression. Reactivated HSV1 has been found to cause inflammatory damage directly, probably involving increased formation of beta amyloid and AD-like P-tau changes found in HSV1-infected cell cultures. HSV1 DNA was found to be specifically localised in amyloid plaques in AD. Further links have been discovered between shared pathways of HSV1 and AD. HSV1 (herpes virus) can cross the blood-brain barrier and remain latent in the brain; combined with carriage of a type 4 allele of the apolipoprotein E gene (APOE-e4), this confers a high risk of developing Alzheimer’s Disease. Some 25-30% of the population carry this gene.
COVID-19 is of particular concern with respect to Alzheimer’s Disease. A pre-existing AD diagnosis is the single highest risk indicator of Covid infection identified thus far; the highest mortality is observed among the most elderly AD patients.
This susceptibility is partly explained by the up-regulation of ACE2R receptors in the limbic regions of AD-affected brains. It is even hypothesised that amyloid-beta is involved in fighting cerebral Covid infection, similar to an observed process with regard to alpha-synuclein in PD and Covid, a defence mechanism that might result in higher levels in the long run.
Reactivation of HSV-1 can aggravate Alzheimer’s Disease processes, such as amyloid beta and p-tau production. It has been shown that Covid can reactivate HSV-1, in particular the S1 spike protein.
Alzheimer’s Disease is viewed as a prion disease, a feature that again puts it into context with Covid-19, a coronavirus whose S1 spike protein has prion-like qualities.
Alzheimer’s Disease is the number one cause for dementia, with no known effective treatments. Finding the ‘root cause’ of this condition in order to produce a targeted cure is further complicated by the fact that the definition of what constitutes AD is somewhat circular. We define the phenomenon by its symptoms:
– Amyloid beta (Ab) plaques: Ab(40-42) oligomers are prominent in AD brains, both in soluble form, where they are more toxic, and in dense plaques, which are thought to serve as reservoirs. These oligomers can cause synaptic dysfunction, dendritic spine damage and neuronal death. Their inflammatory effect includes activation of microglia, astrogliosis, overproduction of cytokines, and dystrophy of neurites. This leads to brain atropy, often first observed in the temporal lobes. The epsilon4 allele of ApoE (e4APOE) is a genetic risk factor thought to affect Ab metabolism; 25-30% of the population have this gene. Ab oligomers can also induce the formation of Neurofibrillary Tangles (NFTs):
– P-Tau: Neurofibrillary tangles of hyperphosphorylated tau (p-tau) is another defining feature of AD. These formations occur after Ab accumulations, though they are seen in frontotemporal dementia without Ab plaques and may also be a parallel, symbiotic phenomenon accelerating disease progression. The Ab / p-tau theory however only accounts for a fraction of the structural dementia comorbidities, and treatment strategies targeting these two aspects have thus far been unsuccessful. This necessitates additional theories:
– Neuroinflammation: While unclear whether this is a consequence or cause of the condition, neuroinflammation is deemed to a major contributor towards the progression and severity of AD, possibly more so than Ab accumulation and NFTs. All three of the above aspects are addressed by another causative, or at least contributory theory:
– Viral Infection: Herpes Simplex Virus (HSV) reactivation is highly correlated with AD; causes damage to the same brain areas that are affected in AD (herpes simplex encephalitis (HSE), induced by HSV, damages the hippocampus, temporal and frontal lobes); is found (by DNA analysis) in substantially all amyloid plaques; is known to alter Ab metabolism, CA2+ homeostasis, synaptic dysfunction and apoptosis in HSV infected neuronal and glial cells. Note that this pertains to carriers of the e4APOE allele, while HSV in the brain of non-e4APOE carriers confers a much lesser risk. At least 80% of the population carries HSV, with only one fifth exhibiting symptoms (e.g. cold sores in times of stress or immunodeficiency); 25-30% of the population carry the e4APOE allele.
The last point is particularly relevant: There are multiple approaches to arresting HSV reactivation (e.g. anti-virals, such as acyclovir, and also components of seaweed(!)), which appears to be the most promising approach addressing suspected cause. It also provides a link with Covid, and an explanation for the high susceptibility of AD patients to this:
Covid, especially the S1 spike protein, has been shown to cross the blood brain barrier (BBB) and enter the brain through a number of pathways, including olfactory and vagus nerve. It has been found to reactivate latent cerebral HSV-1. Amyloid beta (Ab) (1-42) has been found to strengthen the binding of the S1 spike protein of Covid (SARS-CoV-2) to ACE2 receptors and increase viral entry. Covid also increases neuroinflammation. Further, the CA2+ dysregulation in AD facilitates passage of the Covid virus. ACE2 receptors are more prevalent in limbic regions of the brain, including brainstem and hippocampus, and importantly, they are up-regulated in AD brains, thus conferring higher susceptibility. Another possibility is that beta amyloid formation increases in response to HSV (and potentially Covid), as a defence mechanism, resulting in higher aggregation. An analogy is an observation made with influenza viruses, in particular the West Nile Virus, where alpha synuclein production increased to combat the virus (an absence thereof resulted in disastrous disease progression), leading to aggregation and thus higher Parkinson’s Disease susceptibility.
Parkinson’s Disease is the second most common neurodegenerative disorder, after Alzheimer disease (AD).
Onset is usually characterised by motor symptoms: bradykinesia (slowness of movement), rigidity, resting tremor and instability of posture.
REM sleep disorder in Parkinson’s sufferers has been shown to predict worse disease progression. In turn, REM sleep is a function of Default Mode Network deactivation.
With regard to PD, Neurofeedback training has been shown to improve:
– speed of movement initiation
Secondary, non-motor symptoms evolve, such as cognitive impairment, depression, sleep issues (e.g. REM sleep behaviour disorder (RBD), a potential prodromal marker of PD, where paradoxically motor function is improved relative to wake state), and olfactory dysfunction.
Neurofeedback is effective at reducing symptom severity and addressing most of these neuropsychiatric disturbances in healthy patients; while not shown to be a ‘cure’, quality of life improvement can be substantial.
On a cortical level, PD involves the loss of dopaminergic neurons, accumulation of Lewy bodies, damage to neuroglial cells and demyelination of neuronal axons.
Neurofeedback training has been shown to improve myelination across white matter tracts. We can also train frequencies that pertain to glial cells, potentially improving their self-regulation.
A recent study raised the spectre of a connection between COVID-19 infection and Parkinson’s; three persons without familial history developed clinical parkinsonism within 2-5 weeks following infection requiring hospitalisation.
Neurofeedback improves quality of life, sensory integration, motor skills, movement initiation and balance in Parkinson’s Disease.
Peer-reviewed research shows the following effects in neurofeedback applications to Parkinson’s Disease:
– improvement in static and dynamic balance
– improved motor symptoms, on a par with other therapies such as rTMS – while being non-invasive and drug-free
– improvement in life quality
– potential to train up speed of movement initiation by 37%
– increased sensory integration in 10-12 sessions
– reduced symptom severity
General (non-PD specific) effects of neurofeedback training include:
– overall increased fine motor skills
– boost behavioural performance and learning
Comorbid mental health issues, such as anxiety, depression, aggression, and mood imbalances can be addressed directly with neurofeedback.
Chronic Pain is another application for neurofeedback, where studies have demonstrated its efficacy.
Subjectively, PD sufferers find neurofeedback training calming, reassuring and report an improved sense of feeling being part of their body.
It has recently been shown that neurofeedback training led to cognitive improvements in Multiple Sclerosis (MS) patients, and that this corresponded to improved functional connectivity in key motor and salience networks. Increased fractional anisotropy (FA) was observed, which correlated with cognitive improvement.
MS is a neurodegenerative condition that adversely affects axonal myelination. FA is among other a measure of myelination, so the result that neurofeedback can make positive changes in this condition is very encouraging.
Lesions in MS present first in the corpus callosum, a fibre bundle linking left and right brain hemispheres. With a Kaiser Neuromap, we can detect changes in functional connectivity here, which can serve as an early indicator to prompt further investigation at an early stage, while being a complementary approach that is not a substitute for full examination. Neurologists have appreciated this input.
A study with sufferers of Huntington’s Disease, another neurodegenerative condition, showed that cognitive and motor skills improved and that these changes related to improved functional connectivity in key brain regions, again a conclusion that neuroplasticity can be induced despite the presence of neurodegeneration.
The ability of white matter disruption to contribute towards cognitive decline to the extent that dementia results is known since the 1980s when the term “White Matter Dementia” was coined. Various pathologies, including Parkinson’s, Alzheimer’s, Huntington’s, ALD and MS (Multiple Sclerosis) are significantly characterised by white matter disruption. In fact, the involvement of white matter disruption in these neurodegenerative pathologies has been asserted with a certainty that contrasts with the evolution of attempts to define the various ‘diseases’ at times.
Neurofeedback can positively affect white matter growth. In healthy patients, this growth was faster than the rate of neurodegeneration in neurodegenerative conditions. Research has yet to confirm that this works for these conditions specifically.
This approach is non-specific and holistic – we are treating the brain as a whole, and not with regard to a particular condition. Indeed, defining a neurodegenerative pathology is in itself a challenge – Parkinson’s diagnostic criteria have evolved substantially in recent decades and are still subject to debate and expansion, as is the definition of a disease itself. In vivo, that is, before a post mortem examination, Parkinson’s is largely ascertained on the basis of symptoms. It would seem logical to aim therapy at these symptoms, rather than, say, chase a ‘cure’ for an ill-defined phenomenon (is it strictly, and only, dopaminergic neuron death?). This differentiation in approach is important as funding criteria for research into ways to ameliorate the condition often utilise this to the detriment of alternatives. As a result, neurofeedback is sadly neglected in the quest for helping people with neurodegenerative conditions.
Neurofeedback has been shown to help with primary and secondary symptoms in Parkinson’s; it is a non-specific, complementary therapy that is non-invasive and medication-free.
White matter decline is measurable with DTI (Diffusion Tensor Imaging) even before the onset of cognitive decline. The mechanisms by which damage occurs varies by pathology. However any intervention that improves these connections should have a positive effect on the person, both structurally and cognitively. Counteracting this trend in a non-invasive, medication-free and enjoyable manner seems a worthy cause.
The search for a ‘cure’ of different neurodegenerative conditions which lead to dementia is strongly focused on the defining feature – e.g. amyloid beta production in Alzheimer’s, and dopaminergic neurons in Parkinson’s. Addressing symptoms is often seen as a secondary endeavour, with regard to time, prestige, funding and resources. Daniel Webster has spent time working in palliative care and high-support living and rehabilitation facilities. He found that ameliorating life quality can lead to at least a perceived slowdown in the progression of a condition. There is also a possibility that symptom reduction can actually impede a worsening of the condition, and certainly worthy of further research.
Subjective feedback by dementia clients is very encouraging. Research into this aspect of dementia, and how neurofeedback can be applied to slow, arrest and potentially reverse disease progression, is a worthwhile endeavour. Please contact Daniel directly to support initiatives in this regard.
White matter tracts are information superhighways connecting various brain regions and make up c.50% of our brain volume. White matter abnormalities in various forms of dementia, including DLB, Alzheimer’s and Parkinson’s, and mTBI (mild traumatic brain injury) are well documented, and these contribute towards cognitive decline.
With neurofeedback, we can train white matter tracts. This seminal study indicates that we can improve myelination with neurofeedback training. It has been further corroborated since, notably with regard to efficiency.
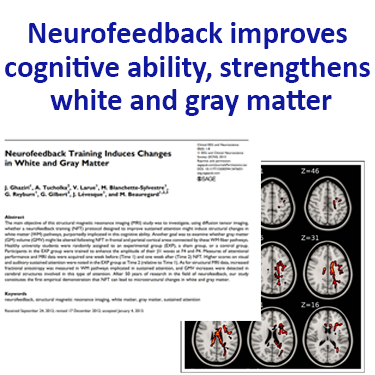
The following account of the recovery of a Stroke patient illustrates the potential efficacy of neurofeedback for Stroke / TBI. For Research on neurofeedback and Stroke / TBI see here.
Claire (name changed) is a 48-year old female who is three years post-thalamic CVA (ruptured aneurysm). In particular, her physical symptoms included severe muscle contractures in her wrist and elbows leading to impaired movement, as well as being wheel-chair bound.
After two neurofeedback sessions, she got her wrist and elbow released.
Claire was getting active elbow extension and shoulder flexion after five sessions. Pain was also resolved in her hand, which had been a major issue previously.
Functionally, she achieved improved independence in dressing skills, required only minimal assistance with bathing, and was able to walk with a cane.
After thirty neurofeedback sessions, Claire started walking without her cane.
Significant improvements (over 50%) included:
– Working memory, chronic aching pain, attention deficit
– night sweats, vertigo and hot flashes
– body awareness, balance, fine motor coordination, muscle spasticity, reflux and chronic nerve pain
– paranoia
Note that this is a subjective account from a therapist and a causal relationship between training and improvements is not proven.
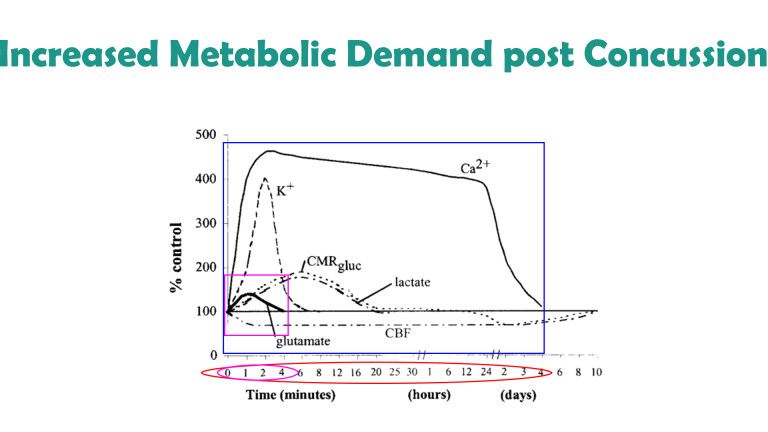
Traumatic Brain Injury (TBI) is another application of neurofeedback training.
We have found neurofeedback to be highly effective in assisting physical rehabilitation. With a Kaiser Neuromap, we can detect areas of hypometabolism that respond hemodynamically with neurofeedback training. There are neuromarkers for mTBI, as well as Alzheimer’s Disease, though these are non-specific (necessary, not sufficient conditions) and should not be seen as diagnosis. General (rather than focal) lesions in neurodegenerative conditions appear to form first in the corpus callosum, a fibre bundle linking the two brain hemispheres; altered functional connectivity has been visible there on a brain map too, in our experience, at an early stage.
There is evidence that neurofeedback supports myelination, improving the important sheathing of axons, which is a critical part of the physical recovery process.
Pain perception has neural correlates – there are brain areas that govern our attentiveness to the signs our bodies are giving us.
In the first instance, these signs are real messages that something is wrong and needs dealing with. Medical attention should provide solutions to this.
Sometimes, pain perception can become irrational in this context, and with neurofeedback training we can help the brain establish a more reasonable approach to interpreting such stimulus.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
Brain Maps and Personalised Brain Training Explained
Personalised Brain Training with Neurofeedback
Neurofeedback lets us train dysrythmic brain areas. With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, short and instantaneously.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the movie; the training process is passive in this sense.
The drop in volume is subtle, so we continue to understand the flow of the movie. No current or electrical stimulation is fed to the brain; sensors simply read brainwaves and the feedback is purely audio-visual.
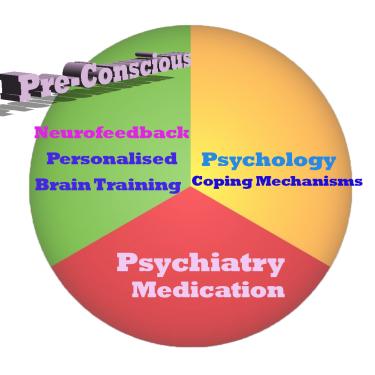
Neurofeedback trains our Pre-Conscious Mind
Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
This equips us with the ability to live in the moment and attain our potential (if we have to resort to conscious control, we are not living in the moment).
We take a holistic approach to healthy brain self-regulation, rather than categorisation or diagnosis.
Personalised Brain Training is an advanced qEEG brain map-based approach to neurofeedback training developed by the founders of the field. Taking Othmer Method / ILF training methods further, it employs Default Network Training protocols as developed by David Kaiser.
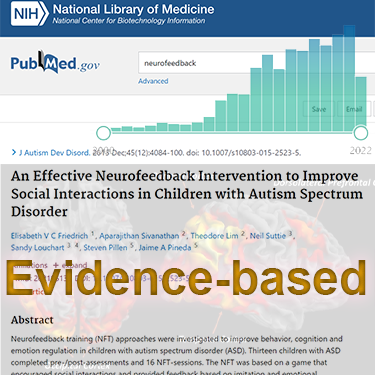
Neurofeedback is Evidence-based
Neurofeedback training is an evidence-based complementary therapy. Its efficacy was first demonstrated some 50 years ago, and with advances in technology, training protocols have become more efficient and the feedback method – watching movies – thoroughly enjoyable.
Neurofeedback is evidence-based. It’s first application was discovered in 1971 when it was used to resolve intractable epilepsy.
There are over 2,000 peer-reviewed research reports on PubMed demonstrating efficacy across a number of pathologies.
In the US, it is an accepted complementary treatment for many challenges.
The Process Explained
Step 1: Brain Map
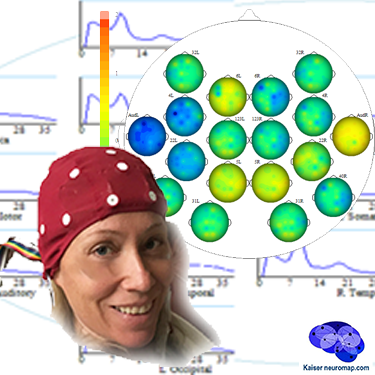
A qEEG recording takes about 45minutes for a 20 minute recording.
A cap with 19 sensors is is fitted to our head and gels inserted to ensure connectivity. The sensors only read – there is a tiny voltage on the surface of our head that these pick up. The gels are easily washed out later. This is also the last time we wear the cap (until a remap after ten sessions); training is done with single sensors.
We analyse the data with Kaiser Neuromap software which gives us a unique view into character traits and vulnerabilities.
Findings are presented in a separate one-hour conversation where we discuss the key elements.
Step 2: Neurofeedback
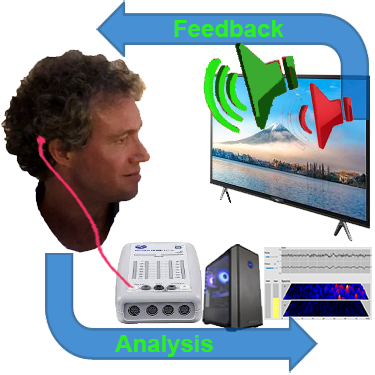
We use a movie of choice as the feedback mechanism – our conscious mind engages with the film, and feedback is delivered by small changes in volume or picture size.
Our pre-conscious mind adapts its behaviour to preserve the more comfortable volume and picture size, and learning occurs.
Volume changes are slight, not stop-start, and the process is enjoyable.
Key is that we are interested in the movie – our conscious mind is engaged with the content, which forms the reward, and our preconscious mind – without our conscious effort – changes its behaviour in response to the feedback.
A two hour training session allows us to do 90-110 minutes of neurofeedback training during which we can work on various brain sites.
This captures an entire ultradian rhythm cycle and corresponds to the approximate duration of feature film movies.
We can start with shorter sessions as appropriate, mainly with children.
Ideally, we do two or more sessions per week to start with.
We would expect to see responsiveness within the first few sessions and remap after twenty hours or about ten sessions.
Generally, we would expect to doing twenty sessions over two months, though this can vary substantially.
We can also accommodate intensives, where we do two sessions per day over a number of days, and have had good results with these.