Нейрофидбэк при расстройствах аутистического спектра (РАС)
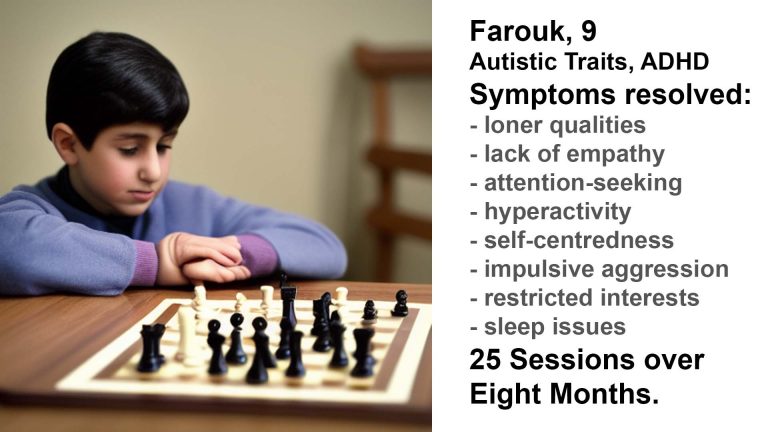
Обратная связь с клиентом
Нейроуправление улучшает симптомы аутизма
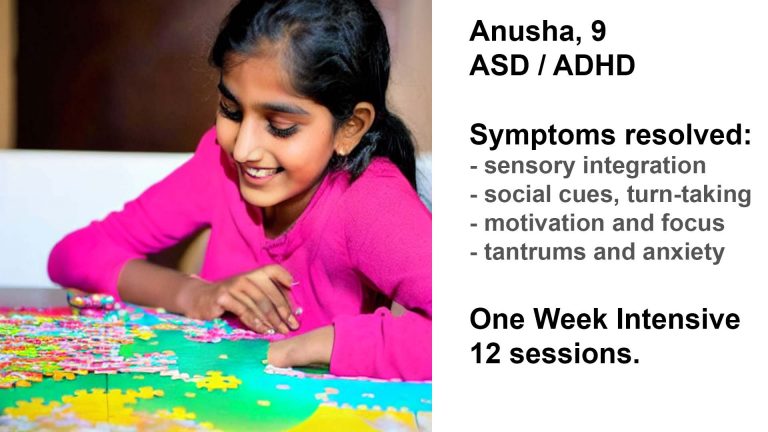
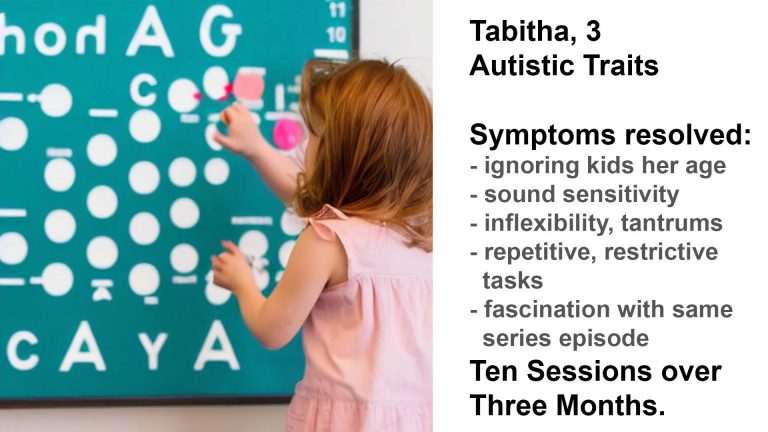
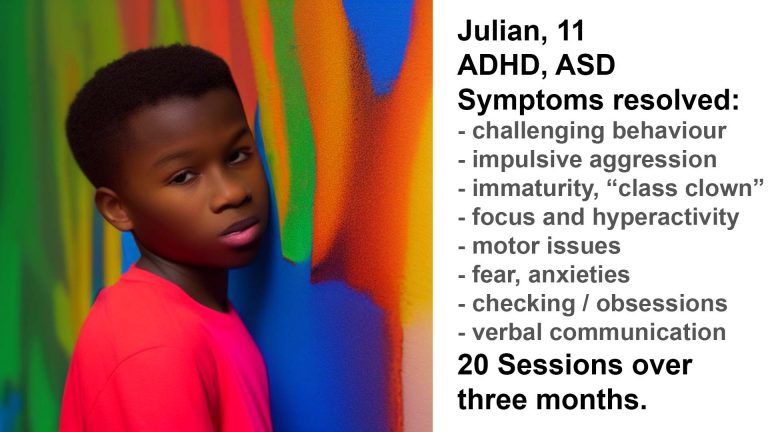
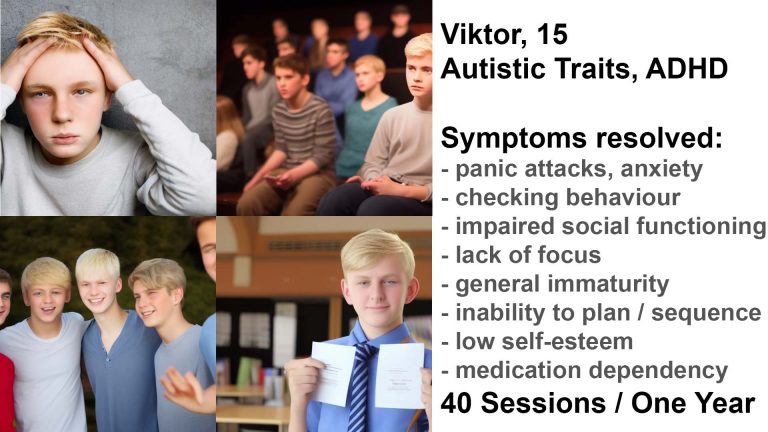
Дэниел Вебстер успешно помог многим аутистам улучшить сенсорную интеграцию, когнитивную гибкость, поведенческие проблемы, а также их способность сотрудничать и заводить друзей. Его подход продемонстрировал ускоренное развитие и улучшения, которые дополняют другие вмешательства.
Он сочетает специальную форму нейробиоуправления со своим обширным практическим опытом работы с людьми всех возрастов в аутистическом спектре.
Этот подход основан на фактических данных, неинвазивн и не требует применения медикаментов.
Изменение траекторий развития
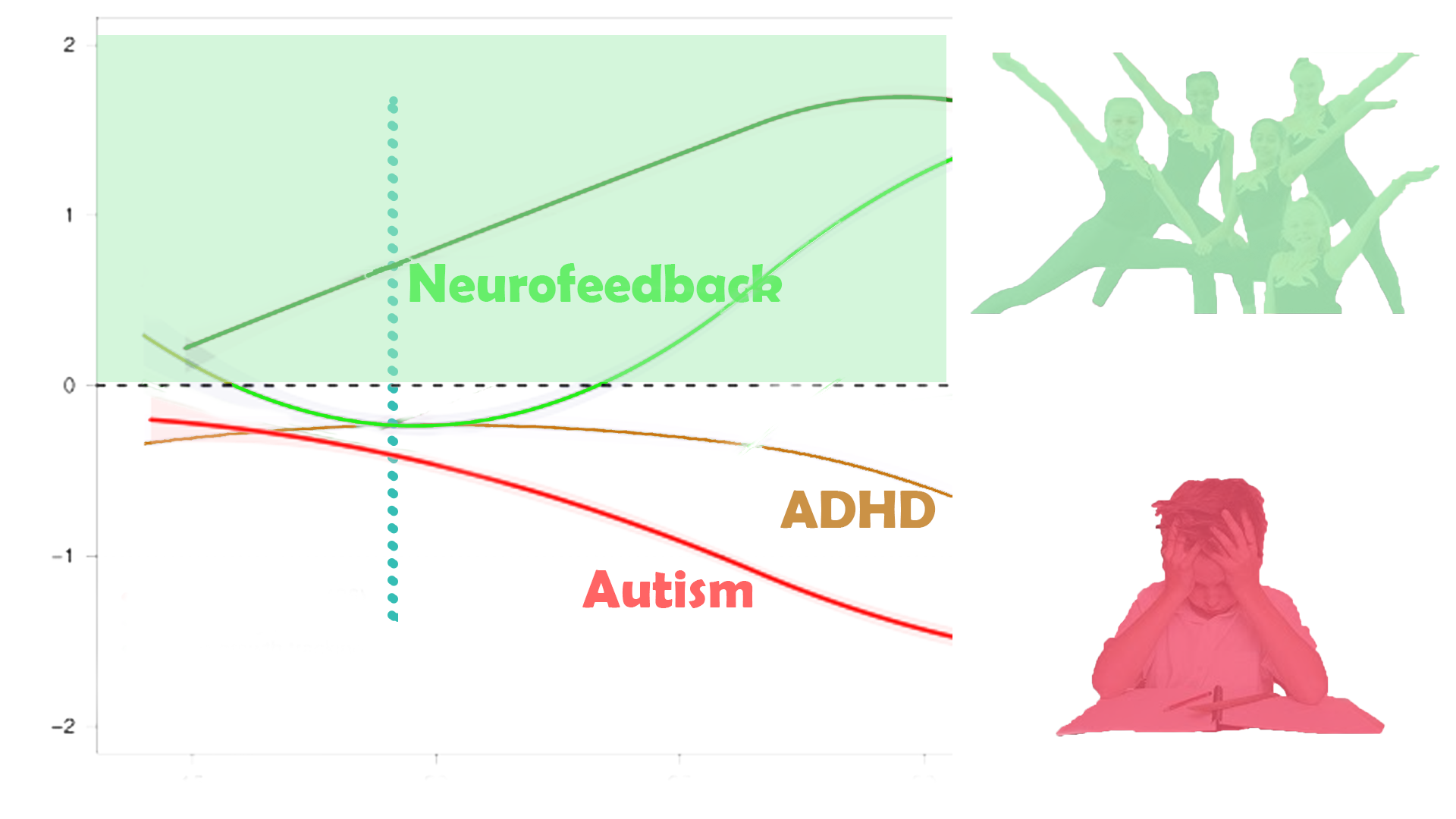
С помощью персонализированной тренировки мозга мы можем изменить траектории развития.
Улучшение сенсорной интеграции, социального функционирования и саморегуляции помогает раскрыть потенциал и способность жить полной жизнью.
Обучение нейробиоуправлению применимо с раннего возраста. Хотя некоторые параметры диагностики утверждают, что аутизм можно оценить только с 3-летнего возраста, признаки могут проявиться гораздо раньше. По нашему опыту, раннее вмешательство может помочь существенно и преобразующе предотвратить развитие событий (см. тематические исследования).
По оценкам, 15-40% случаев РАС считаются регрессивными, когда нормальное развитие до 15-19 месяцев сопровождается потерей словарного запаса, снижением социального взаимодействия и реакции, а иногда и повторяющимся игровым поведением. Мы не занимаемся диагностикой.
В результате усилия и затраты на уход в будущем часто могут быть существенно сокращены. Средняя стоимость поддержки аутичного человека в течение всей жизни оценивается в 3,2 миллиона долларов. Для сравнения, обучение нейробиоуправлению, хотя и требует больших затрат, является лишь частью этого.
Обеспечение более широкого проявления талантов может привести к увеличению потенциального дохода и финансовой самодостаточности. Эти «дивиденды» со временем материализуются, и их текущая стоимость может во много раз превысить инвестиции, сделанные в персонализированную тренировку мозга на более раннем этапе.
Например, высокофункциональный взрослый человек с РАС может пользоваться структурированным дневным уходом в доме престарелых или в дополнение к нему. Другая возможность заключается в том, что поддерживаемый образ жизни либо не подходит, и они живут со своими основными опекунами (например, родителями), что увеличивает их финансовое бремя. Изменение их траектории путем улучшения социальных навыков и связанных с ними проблем психического здоровья может помочь им попасть на структурированное рабочее место, повысив их самооценку и уверенность, а также обеспечив им доход.
Подобные вмешательства могут значительно улучшить качество жизни. Повышение независимости, самореализации и самовыражения, а также поддержание друзей и социального взаимодействия являются неизмеримыми дополнениями к жизни уязвимого человека.
Обучение нейробиоуправлению является неинвазивным и не требует медикаментозного лечения, и этот органический подход к лечению уважает выбор человека.
Тематические исследования
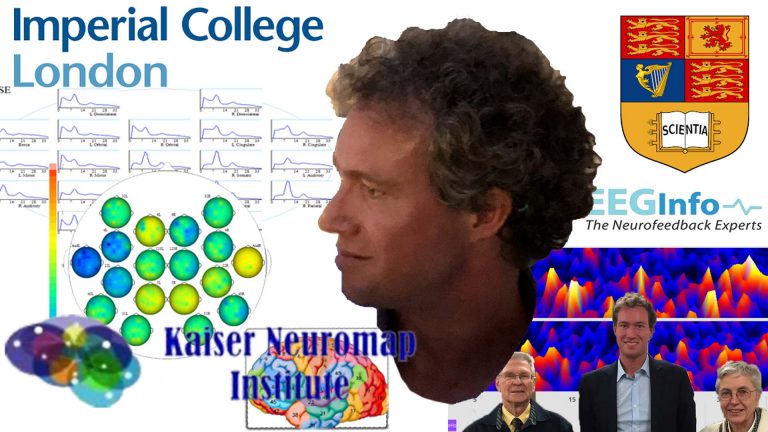
Дэниел Вебстер использует самую сложную и содержательную методологию интерпретации qEEG, чтобы выявить индивидуальные проблемы и сформировать план обучения нейробиоуправлению.
Выявление индивидуальных проблем с помощью карт мозга qEEG
Дэниел Вебстер использует самую сложную и содержательную методологию интерпретации qEEG, чтобы выявить индивидуальные проблемы и сформировать план обучения нейробиоуправлению.
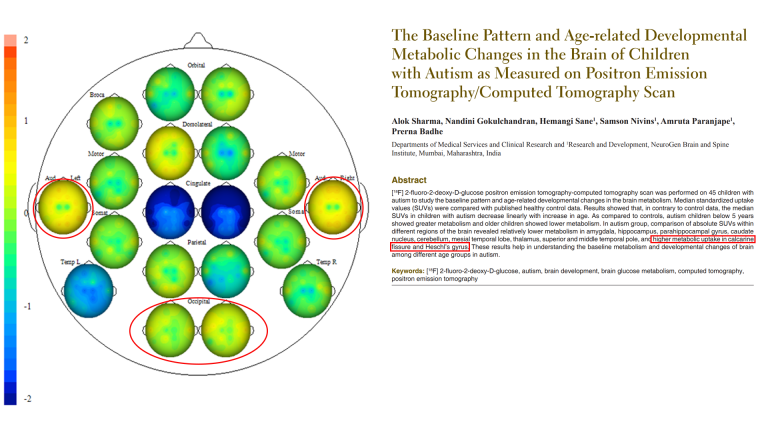
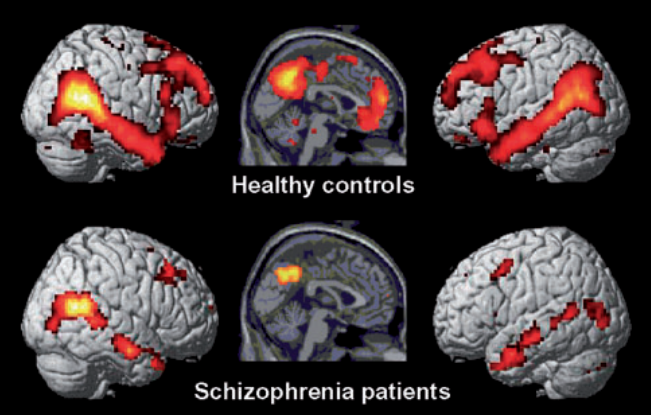
Идея изучения мозга для выявления проблем кажется интуитивной. И только в этом тысячелетии такой подход стал реальным. Методики интерпретации карт мозга сильно различаются. Дэниел использует метод, который позволяет нам оценить зрелость областей Бродмана, чтобы получить детальное представление о функциональных связях — о том, как отдельные области мозга взаимодействуют друг с другом. Это позволяет нам увидеть, в чем заключаются проблемы с сенсорной интеграцией, сетевой интеграцией, социальной зрелостью мозга и многими другими поведенческими аспектами. Исследования функций зон Бродмана в настоящее время изобилуют более чем 200 отчетами PubMed в год. Погрузившись в эту захватывающую область, мы находим нейромаркеры моделей поведения в результате научных исследований фМРТ, которые подтверждают результаты нашей технологии карт мозга.
Важно отметить, что этот подход позволяет нам связать поведение с физиологией, а не, скажем, с устаревшими психологическими моделями. Тренируя те части мозга, которые, по нашему мнению, аритмичны, мы можем ускорить зрелость с помощью передовых методов нейробиоуправления, которые использует Дэниел. Результаты воспринимаются когнитивно, и повторные карты подтверждают этот прогресс.
Сенсорная обработка и интеграция
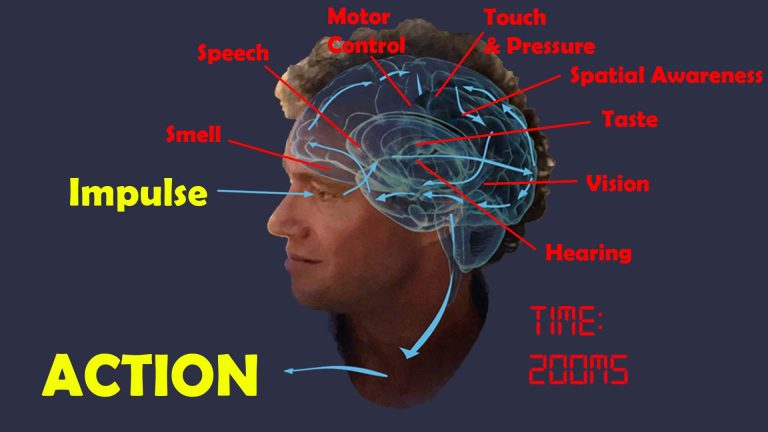
Определенные области мозга обрабатывают сенсорную информацию
Наш мозг – хранитель наших чувств. Он управляет нашей чувствительностью и структурирует наши реакции. Проблемы сенсорной обработки и интеграции при аутизме (и любой другой патологии) в значительной степени контролируются нашим мозгом. Таким образом, имеет смысл тренировать способность нашего мозга различать, обрабатывать, интегрировать и контролировать поток информации, генерируемый сенсорными стимулами.
Движение, координация и действия также управляются нашим мозгом. Фактически, функции более высокого уровня в областях нашего мозга, отвечающих за обработку двигательных навыков, также регулируют наше понимание социальных границ и личного пространства.
Существуют отдельные области мозга, которые интерпретируют соответствующие сенсорные сигналы, и посредством различных этапов конвергентной обработки — областей мультимодальных ассоциаций — мозг конструирует сцену и понимает, где мы находимся относительно окружающей среды. Например, задняя или затылочная область нашего мозга — это место, где анализируется визуальная информация; Слуховая обработка происходит в височной доле, рядом с нашими ушами.
Когда какая-либо из этих областей мозга становится аритмичной, наша интерпретация искажается, например, мы можем стать гипер- или гипочувствительными, как это видно при различных симптомах аутизма.
Индивидуальная чувствительность существенно различается. С помощью карты мозга мы можем определить, какие именно области сенсорной обработки уязвимы, обеспечивая персонализированный подход.
С помощью нейробиоуправления мы можем тренировать области мозга, отвечающие за эффективную обработку и интеграцию сенсорной информации. Повышенная чувствительность к звуку, а также излишне эмоциональная интерпретация сказанного становятся утонченными и гибкими. Улучшается осознание тела и контроль движений, а также распознавание лиц. Это основано на фактических данных и подтверждено результатами нашего обучения.
Наш мозг предсказывает поведение
Сенсорная обработка требует времени. От воспринимаемого импульса, например визуального ввода, до решения и двигательного действия, это может занять до 200 мс, или одну пятую секунды. Чтобы компенсировать задержку между восприятием и реальностью, нашему мозгу необходимо заниматься прогнозирующим поведением. По сути, мы моделируем окружающую среду и подтверждаем предсказания нашими органами чувств.
На базовом уровне это позволяет нам предвидеть, где будет находиться движущийся объект, например приближающийся теннисный мяч, и соответствующим образом планировать действия. Если бы мы полагались исключительно на реакцию на стимулы, которые регистрируются нашими органами чувств, мы бы пропустили мяч или любой другой приближающийся объект.
На более высоком уровне мы применяем эту способность прогнозного моделирования к моделям поведения, включая людей вокруг нас, а также к событиям и последствиям действий в целом.
При аутизме способность моделировать и прогнозировать нарушена или недостаточно развита. Степень этой неспособности варьируется в зависимости от человека. В результате мир представляет собой постоянную новизну, которая может быть как увлекательной, так и сбивающей с толку. Появляется предпочтение предсказуемого поведения, распорядка дня и повторяющихся ограничительных действий. Хотя это может привести к появлению сильных сторон и специализации, это также является недостатком при взаимодействии с другими людьми или нахождении в меняющейся среде.
Улучшение возможностей моделирования и прогнозирования с помощью нейробиоуправления Дэниела основано на двух подходах:
1. развитие и созревание отдельных областей сенсорной обработки, руководствуясь картой мозга, с учетом индивидуальных различий.
2. усиление сетевых связей, то есть взаимодействия между областями мозга, которые объединяют обработанную сенсорную информацию и определяют наше самоощущение и внимательность к окружающей среде, включая различные сети (сеть режима по умолчанию, сеть значимости, сеть позитивных задач / центральный исполнительный директор). Сеть, система зеркальных нейронов).
Мы делаем это, тренируя отдельные участки, а также различные средства связи, посредством простого процесса привлечения сознательного разума к награде – фильму – одновременно давая предсознательным областям обратную связь о различных протоколах тренировки, слегка уменьшая громкость – но все еще слышно – и временно – доли секунды – когда определенные частотные характеристики не соблюдаются. Повторение показывает мозгу более эффективную модель поведения, которую он будет стремиться перенять. Таким образом, обучение является пассивным и органичным.
Персонализированная тренировка мозга использует самый передовой метод интерпретации карт мозга qEEG для формирования индивидуального плана тренировки. В нашем методе нейробиоуправления применяются наиболее эффективные протоколы обучения с приятным процессом обратной связи и просмотром фильмов по выбору.
Уважение индивидуальности при аутизме
Важно быть сострадательным и непредвзятым, поэтому нам необходимо отказаться от стандартов, по которым мы оцениваем нейротипическое поведение и сопереживаем человеку с РАС: измененная сенсорная интерпретация может вызвать крайние реакции; снижение способности планировать, организовывать и выполнять задачу может привести к нестабильной работе; социальные навыки, возможно, нуждаются в большей практике, равно как и понимание границ, правил и личного пространства; Поведение, направленное на поиск стимулов, может показаться необычным, но правдоподобным в контексте индивидуальной системы вознаграждения человека.
Их могут шокировать взгляды, с которыми они сами не сталкивались и которые не могут принять/терпеть/осмыслить; аспекты внешности другого могут отпугнуть их, но при этом не являются злонамеренными; очередность может дезориентировать и нарушить их предпочтение собственным правилам и процедурам; неожиданные взгляды/действия могут их отпугнуть и вызвать враждебность там, где это не было запланировано.
Изменения могут представлять собой нежелательную сенсорную/процессорную перегрузку, с которой они не готовы справиться, вызывая тревогу и чувство враждебности; адаптация к новым ситуациям может перегрузить их способность определять последовательность действий, моделировать новые результаты и сохранять мотивацию; это может создать ощущение невзгод и отсутствия принятия, воспринимаемое слишком лично и влияющее на самооценку и уверенность, особенно когда для освоения рутины требуется время и она связана с определенными результатами вознаграждения.
Определенное поведение может быть реакцией на форму сенсорной перегрузки, и его неочевидно обнаружить/осмыслить до тех пор, пока вы не начнете лучше сопереживать или узнавать человека и оценивать контекст, в котором он прибегает к рассматриваемому поведению. Они могут защищаться или быть приучены к достижению чего-то таким способом, когда есть другие альтернативы, которым можно научить.
Персонализированная тренировка мозга предполагает оценку индивидуальных сенсорных уязвимостей каждого человека с помощью карты мозга.
Социальное функционирование
Заводить друзей и создавать союзы — это качество млекопитающих, которое наиболее выражено у людей и позволяет нам достигать исключительных достижений в построении цивилизации, которых мы не могли бы достичь самостоятельно. Социальное функционирование является ключевым компонентом этого, и мы можем помочь людям с аутистическим спектром существенно улучшить это качество.
Признание и оценка способности другого человека к независимому мышлению и масштабу действий является фундаментальным компонентом социального взаимодействия, называемым Теорией разума.
У нас есть префронтальные области мозга, которые управляют чувством социальных правил и различиями между собой и другими. Человеческое взаимодействие также определяется границами: социальная граница одного человека — это личное пространство другого, и наоборот; мы процветаем, когда находим подходящий уровень агрессивности и возможности вербовки. Невпускание людей в свое личное пространство, т. е. чрезмерное упрямство, создает границы, а чрезмерная агрессивность отталкивает и считается неуважением. В этом есть культурные компоненты, создающие вариативность, и, как всегда, гибкость является ключевым моментом. Обе характеристики — социальные границы и личное пространство — управляются отдельными участками мозга, которые мы можем тренировать.
Наша система миррон-нейронов позволяет нам быстро изучать действия и поведение на основе наблюдения. Это хорошо изученный набор нейронных узлов или отдельных областей мозга, который лежит в основе социально-когнитивных процессов подражания, эмпатии и теории разума. Мы можем тренировать эти области и их сплоченность с помощью нейробиоуправления неинвазивным и безмедикаментозным способом.
Социальные эмоции распознаются и обрабатываются отдельными областями мозга. Когда они аритмичны, может возникнуть целый спектр симптомов. Восприятие находится на переднем плане, и наша система зеркальных нейронов играет ключевую роль в этом. Предполагая здесь некоторую функциональность, мы тогда можем увидеть возможную предвзятость эгоцентризма, означающую, что мы склонны выносить эмпатические суждения, основанные на нашем собственном состоянии ума, игнорируя при этом другого. Это также может отрицательно повлиять на нашу способность переключать внимание и распознавать свободу действий. В результате возникают трения с окружающей средой и один из факторов социальной тревожности. По нашему опыту, тренировка этих областей мозга приводит к значительному успокоению и принятию.
Признание потребностей других людей и их удовлетворение таким образом, чтобы сохранить наши собственные потребности и амбиции, является ключом к плавному социальному взаимодействию, такому как очередность. Мы полагаемся на стабильное и развитое самоощущение, которое обеспечивает наша сеть режима по умолчанию и ее здоровое взаимодействие с нашей сетью позитивных задач. Основная часть нейробиоуправления Дэниела — это его тренировка в рамках целостного подхода.
Ослабление тревожности и уменьшение фобий — это научно обоснованный эффект персонализированной тренировки мозга. Существует множество корковых источников тревоги. Это может принимать форму социальной тревоги, когда человек не понимает социальных сложностей или эмоций; тревога «что дальше», когда мы не уверены в своем отношении к происходящему перед нами; реляционное мышление, при котором мы запрограммированы думать, что все сенсорные стимулы направлены на нас, и не можем чувствовать себя достаточно отстраненными; или чрезмерная забота о своей внешности. Фобии могут проявляться негибкостью при столкновении с ситуациями, напоминающими предыдущую неприятную ситуацию. Они также могут быть результатом сенсорной перегрузки или отсутствия обработки/интеграции, например, в отношении звука, высоты, света, вкуса или осязания. И снова мы находим эту решимость благодаря тренировке Дэниела по нейробиоуправлению.
При аутизме часто ухудшаются способности к прогнозированию. Это может включать в себя неспособность поймать мяч или предвидеть движение объектов в целом, что часто является опасным недостатком во внешнем мире. Это также распространяется на моделирование поведения и потребностей других, ухудшая нашу способность проявлять внимание и интегрироваться в более сложные социальные ситуации. Еще одним частым проявлением является негибкость в отношении распорядка дня и усвоенного поведения. На более тонком уровне нарушение способности прогнозировать может привести к неправильному пониманию несоответствий, восприятию вещей слишком буквально и, таким образом, к неспособности оценить юмор, иронию или сатиру. Это, в свою очередь, может привести к недоразумениям, которые вызывают трения с окружающей средой. Наша сеть режима по умолчанию играет здесь важную роль, и мы можем ее обучить, чтобы значительно улучшить качество жизни во многих аспектах.
Социальные правила являются важной частью социального взаимодействия. Они могут быть неявными и могут включать исключения, требующие неполяризованного подхода, специфичного для конкретной ситуации. Мы можем тренировать эту гибкость как в отношении восприятия, так и в отношении манипулирования.
Вербальное и невербальное общение — сложная тема, которой посвящен этот раздел; мы часто обнаруживаем существенные скачки в тандемном повышении мотивации и самооценки, возникающие в результате развития вышеупомянутых аспектов.
Саморегулирование
Общими чертами людей с аутистическим спектром являются страх неожиданных действий и последствий; неспособность моделировать окружающую среду и абстрагировать новые впечатления; и чрезмерное упрямство, перерастающее в импульсивную агрессию и часто в ярость.
Страх и тревога имеют нейронные корреляты, которые обычно не регулируются у аутичных детей и взрослых. Некоторые из них пересекаются с проблемами сенсорной интеграции, а тренировка соответствующих областей мозга обеспечивает значительное успокоение.
Наше самоощущение управляется нашей сетью режима по умолчанию — набором областей мозга, которые обеспечивают нейронную основу «я» и активируются во время самореферентного мышления, мечтаний и воображения. Активность этой сети снижается, когда мы вовлечены в окружающую среду, уступая место сайтам Task Positive Network. Наша способность гибко активировать и деактивировать каждую из этих сетей различным образом является ключом к оптимальной производительности. Когда этот процесс не регулируется, возникают проблемы с социальным функционированием, а также с компульсивным поведением. Проблемы сенсорной интеграции усугубляют эту тенденцию, и мы видим повторяющиеся, ограничительные модели поведения, которые, по-видимому, обеспечивают успокоение и передышку за счет отстраненности от нашего социального окружения.
Другие основные сайты DMN управляют нашей способностью самоуспокаиваться и заботиться о себе, то есть как обеспечивать рациональный способ отговаривать себя от ситуаций, так и создавать эмоционально безопасную среду. Это влияет на контроль настроения, импульсивность, качество сна, эмпатию и дифференциацию себя и других.
В мире, который постоянно меняется, рутина и предсказуемость дают передышку. С помощью нейробиоуправления мы помогаем разными способами:
– уменьшить страх, слуховую чувствительность и тревогу
– укрепить ключевые функции мозговой сети для улучшения прогнозирующих способностей и способностей к абстракции.
– уменьшить склонность к импульсивной агрессии и дальнейшей ярости, когда результаты не соответствуют ожиданиям
– восстановить/создать способность к самоуспокоению и самовоспитанию
– улучшить планирование, концентрацию и мотивацию
– тренировать способность различать себя и других, осознавать социальные границы, восприятие других и социальных эмоций.
Повышенная гибкость приводит к ускоренному взрослению и самореализации.
Мы успешно обучили соответствующие области мозга восстановлению чувства заземления. Поведенческие изменения обычно заметны уже через десять сеансов. Одновременно мы видим и ощущаем облегчение и новую гибкость, которая освобождает как человека, так и его опекунов/опекунов. Примеры см. в тематических исследованиях.
Речь и язык
Каждый четвертый человек с РАС невербальный, и 40% всех детей, направленных в клинику аутизма, имеют значительную задержку речи, независимо от диагноза.
Младенцы начинают понимать и производить отдельные слова и жесты в контексте игрового взаимодействия с 12-месячного возраста; в период 18-24 месяцев происходит быстрое расширение словарного запаса и знание правил разговорного обмена. Обычно развивающиеся дети используют язык для социального взаимодействия; это контрастирует с детьми с РАС, которые чаще используют слова для регулирования своего окружения (требования, протест), а не с коммуникативными намерениями. Несмотря на широкий диапазон языковых способностей, навыки артикуляции обычно не развиты. Существует сильная связь между языком и социальными навыками при аутизме.
Речевое развитие имеет множество компонентов, каждый из которых имеет нейронные корреляты, а это означает, что существуют области мозга, способствующие пониманию и воспроизведению языка, которые должны созреть и эффективно работать вместе. Это означает, что у нас есть шанс улучшить генерацию речи путем тренировки мозга, и исследования и опыт подтверждают это. Приведенное ниже исследование показывает, как мы можем помочь улучшить необходимые строительные блоки, которые способствуют развитию речевых и языковых способностей человека.
Речевое и языковое развитие также является функцией социальной взаимности, как в отношении инициации, так и в отношении восприятия. Поэтому его следует рассматривать не изолированно, а скорее как сопутствующий компонент улучшения эффективной синхронизации с социальной средой.
Персонализированная тренировка мозга использует целостный подход к улучшению социальной интеграции посредством тренировки различных функций познания и сознания, включая самоощущение, совместное внимание, теорию разума, концентрацию, регуляцию настроения, поведенческие проблемы и общение, как вербальное, так и невербальное. .
Научные данные: нейробиоуправление при аутизме
Было доказано, что обучение нейробиоуправлению является безопасным, выполнимым и эффективным подходом к терапии расстройств аутистического спектра в любом возрасте.
Многочисленные исследования подтверждают:
– Улучшение когнитивных функций в социальной сфере, мышлении и внимании.
– улучшение когнитивной гибкости
– снижение стимулирования, улучшение речевой и языковой компетентности, использование воображаемых игр
– стойкое улучшение исполнительных функций, рабочей памяти и скорости обработки информации
– улучшенное распознавание лиц
– лучшее поведение, в том числе менее агрессивное, более склонное к сотрудничеству и более эффективное общение.
– улучшенная функциональная связь в социальных областях мозга
– снижение симптомов РАС на 40% у 89% участников и связанные с этим изменения в функциональных связях головного мозга.
– длительное улучшение гибкости ACC/DMN, критически связанное с теорией разума
– значительные улучшения в общем и невербальном общении и социальном взаимодействии
– устойчивые и растущие улучшения после периода обучения в контроле внимания, когнитивной гибкости, планировании, общении и социальном взаимодействии.
В крупномасштабном исследовании сообщалось об улучшении IQ на 9 пунктов, а также об уменьшении симптомов РАС, включая внимание, тревогу, апросодии, социальное функционирование, а также академическое и интеллектуальное функционирование.
У детей улучшилось сенсомоторное поведение (постурография).
Тренировка нейробиоуправления доказала свою успокаивающую эффективность.
Научные данные о сопутствующих заболеваниях, например. СДВГ, дислексия, депрессия, тревога, судороги, сон и поведение показаны на соответствующих вкладках ниже.
Autism: Related Mental Health Issues
A brain map lets us look into our brain – how the different parts communicate with eath other. With neurofeedback, we can train optimal integration.
The following tabs describe how Personalised Brain Training can help resolve many mental health issues in a holistic, non-invasive and medication-free manner.
(Scroll down on mobile)
We can think of autism as brain dysregulation in multiple functional areas. This results in many comorbidities, which we implicitly address with neurofeedback training as part of a holistic approach.
Some of the challenges we have seen to improve with neurofeedback training include:
– lack of bodily awareness, motion control and speech, spatial awareness
– an inability to express, understand and convey emotions and physical needs
– increased frustration at not being understood, whether on a basic survival needs level or in more emotional / intellectual areas
– impulsive aggression, potentially morphing into self-fuelling rage and violent behaviour, sometimes self-directed
– perceived lack of empathy and regard for the needs of others
– generally being ‘misunderstood’, to the detriment being able to fully develop strengths and talents
With neurofeedback training, we can address these ultimately self-harming divergences and bring out the incredible potential in all of us.
(Scroll down on mobile)
ADHD, Focus & Planning
The vernacular description of ADHD has come to include many other issues than its core definition of distractibility and/or hyperactivity. We often find many other comorbidities, such as behaviour problems, impulsive aggression, rage, excessive stubbornness, various anxieties, mood dysregulation, sleep problems, dyslexia and inappropriate social skills.
With a brain map, we can assess vulnerability to a host of other possible issues, and then address these with neurofeedback training in a personalised manner. Furthermore, we have a chance at promoting structural improvements, such as prefrontal brain maturity. The core issue of ADHD, Distractibility, is dealt with here:
Focus and Productivity have three core components:
– Concentration
– Planning and Organisation
– Motivation
Each of these three components is governed by a different brain area. When one or more of these regions is dysrhythmic, we are vulnerable to focus issues.
– Planning and Organisation: understanding goals, working back to the present and structuring a workflow conducive to achievement, seeing the bigger picture and dividing projects into tasks, prioritising these and being flexible.
The ability to form an overview of the task at hand, break this down into smaller, manageable steps, and sequence these accordingly, can be trained.
– Concentration: the ability not to be distracted and maintain attention on the relevant task at hand. Distractibility is a function of spatial awareness, and there are brain areas dedicated to this task. When they are dysrythmic, we become easily distracted.
– Motivation: having sufficient drive, optimism, persistence and endurance to implement plans and overcome setbacks. Self-esteem, an understanding of one’s own strengths and weaknesses, and the ability to self-soothe, that is, to rationalise thoughts, are key to this.
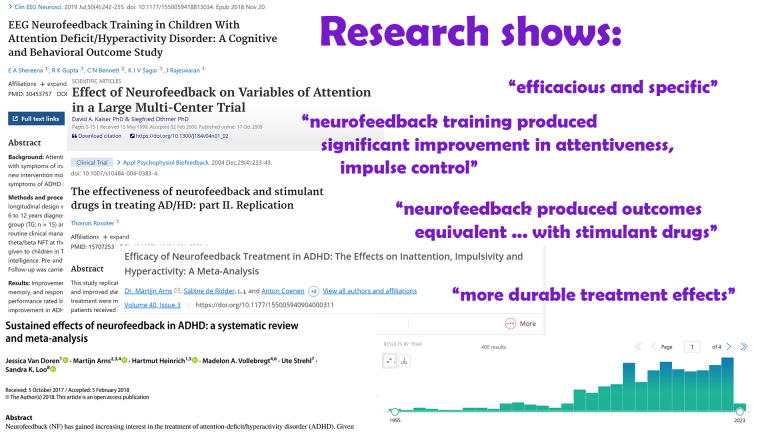
Researchers conclude that neurofeedback training can be considered “Efficaceous and Specific” (Level 5) for ADD / ADHD. Neurofeedback training was shown to produce significant improvement in attentiveness and impulse control. It was shown to produce outcomes equivalent to those obtained with stimulant drugs. The effects were shown to be long lasting.
Neurofeedback and ADHD Medication
We have successfully helped children and teenagers reduce or discontinue stimulant medication treatment of ADHD where this has become undesirable, under supervision of the prescribing entity.
Individuals may offer motivations to change stimulant medication use to alternate forms of therapy, including ambiguity concerning long-term use and reduction of symptom-severity effectiveness at the cost of growth (height). Many are considered “prohibited substance” in competitive sports, being listed as Schedule II / Class B substances when obtained without prescription. Possible sleep problems are documented.
There appears to be a range of conclusions in studies regarding the effect of psychostimulants used to treat ADHD on mood, anxiety, emotional reactivity, substance abuse, psychiatric conditions, cardiovascular implications, tics and other dyskenisias, among other, and these vary considerably in sample size, duration and scope.
A study with over 130 participants showed that neurofeedback can be used effectively in combination with pharmacological treatment, enhancing results.
See here for more information.
Research on Neurofeedback and ADHD
Neurofeedback training for ADHD is evidence based and produces lasting results:
Attention deficit: Efficacy is well-documented – there are over 370 research reports on Neurofeedback and ADHD on PubMed.
In line with AAPB and ISNR guidelines for rating clinical efficacy, neurofeedback can be considered “Efficacious and Specific”, the highest level (5), with a large effect size for inattention and impulsivity in this study.
A large-scale study showed that neurofeedback is effective in remediating attentional dysfunction. Significant clinical improvement in one or more of attentiveness, impulse control, and response variability was observed in 85% of participants after 20-40 training sessions.
Impulse control and attention improved through neurofeedback training, producing “patient outcomes equivalent to those obtained with stimulant drugs”
Neurofeedback “appears to have more durable treatment effects, for at least 6 months following treatment.”
Neurofeedback was shown to be an effective method to enhance cognitive deficits, reduce ADHD symptoms and behaviour problems in children. The effect was maintained in a follow-up six months later.
There are numerous academic studies confirming the efficacy of EEG biofeedback (another name for neurofeedback) with sustained performance gains.
The American Academy of Pediatrics bases its conclusion that there are “no significant contraindications” to its use on these studies.
ILF / Othmer Method neurofeedback training was shown to reduce ADHD symptoms, specifically distractibility and impulsiveness, in a study involving 251 children over a course of 30 neurofeedback sessions.
Training specific brain areassuccessfully activated error monitoring networks in ADHD patients, associated with symptom improvements. Dynamic functional connectivity was found to be maintained in a follow-up 11 months later.
Another study attested improved response control and attention in ADHD post Neurofeedback.
Mood regulation and Motivation: see here
Working Memory: see here
Sense of Self: With Personalised Brain Training, we work on the Default Mode Network, the neural basis of self.
Challenging Behaviour, Anger, Aggression, Rage
Lack of mood regulation, self awareness, and inhibitory control contribute to anger management and behavioural issues. These complicated behaviour patterns have a neural basis and vary by individual. With a Kaiser Neuromap we can detect vulnerabilities and train these with neurofeedback.
Excessive obstinacy, misunderstanding social cues and general overwhelm and anxiety are frequent characteristics of autistic children. With neurofeedback training, we have had success in remediating these symptoms.
Multiple brain areas contribute to impulsive aggression, self-fuelling rage, physiological arousal, ‘acting out’ and conversely calming down and rationally understanding one’s behaviour and even showing regret, remorse, understanding and insight, or not as the case may be.
A Kaiser Neuromap shows us possible vulnerabilities to such behaviour patterns, and can help us form a more nuanced understanding of a person’s preconscious drivers, that is, their ‘wiring’. There are multiple contributors which we can address:
– impulsive aggression, e.g. in response to being denied something
– rage, a continued unconsolable stage
– lack of empathy or understanding of others’ feelings
– inability to see different perspectives
– turn taking, self/other differentiation, shared authority
– monitoring and understanding consequences of actions
With neurofeedback training we can work on these preconscious processes, which occur before a person is able to apply conscious control or inhibition. The aim is to reduce or eliminate the person’s propensity to exhibit such adverse and undesirable behaviour in the first place, freeing up the mind to enjoy the moment in constructive synchrony with others.
Neurofeedback helps us stabilise the Default Mode Network, and reduce impulsive aggression and physiological arousal control. We have seen success within a few sessions in clients from 8-15 years of age.
Anxiety and Fear
There are many manifestations of anxiety, including social anxiety, panic attacks, excess body awareness (body dysmorphia), emotional hypersensitivity, fears and phobias. Autistic children generally present with a variety of these, all contributing towards an energy-consuming heightened state of vigilance. Stress and defensive behaviour results.
Neurofeedback is an established, evidence-based treatment for anxiety.
It was found that neurofeedback training for anxiety and depression “results in enduring improvements approximately 80% of the time”
Confidence and social integration tend to improve accordingly, resulting in a positive feedback loop that helps shape new trajectories.
A brain map will reveal overactivity of brain areas responsible for monitoring consequences of actions (timidity, general fright and reticence); watching out for an abuser (bully); body and face awareness; and excessive self-monitoring. This helps us understand the potential presence of real threats and fear factors. We can also detect possible tendencies to develop unhealthy body awareness. Neurofeedback training lets us address this issues.

There are multiple types of anxiety, each correlating with one or more brain areas being dysrhythmic:
Social anxiety: When we’re in a situation with other people and our understanding of the social dynamics and complexities is overwhelmed.
Sensory overload: our brain interprets all sensory stimulus as directed to ourselves. We lose the ability to discern what is directed at us, and which matters or interactions are of no concern to us. This sets us up for panic attacks and ultimately psychosis. It also means we become singular in our perspective, unable to take on other points of view
Loss of narrative: Our episodic understanding of the situation, how we got there and what happens next, is impaired, and we are unsure of where we are and where we’re going. This hyperactivates our amygdala, and the sensation is highly emotional
Auditory sensitivity: we become prone to overly interpreting the emotional content of words and sounds, creating an air of prickliness and pushing people away without knowing it
Activation: Our ARAS is responsible for setting the right level of physiological arousal, or wakefulness, for the situation, and to remain stable there. When this is on overdrive, we are pushed further into fight-or-flight mode than necessary, thus heightening sensory sensitivity. Panic attacks are an extreme manifestation. Our ability to calm down quickly is reduced.
Trauma: an inability to self-nurture – creating an emotional safe-space around us – and self-soothe – being able to talk ourselves down rationally from a situation, thus resulting in mood instability. This can also manifest in dissociation and heightened pain perception. We ruminate about the past and worry about the future, instead of being able to enjoy the present.
Intrusive thoughts: Self-criticism overshadows motivation and confidence, and we become self-aware and distracted by negative thoughts and feelings. Some use acquired habits to distract from this. Others become attached to the reward circuitry triggered, and sustained by feeding obstructive, self-deprecating thought content. Our confidence, motivation and social interaction suffer as a result.
Neurofeedback for Autism
Autism is a spectrum disorder characterised by social integration issues and developmental delays that can be both physical and emotional. With a Kaiser Neuromap we can identify individual weaknesses, and train these with Personalised Brain Training in a non-invasive, medication-free manner. Improvements are evidence-based and impressive.
There are distinct brain areas that interpret the respective sensory input, and through various convergent processing stages – multi-modal association areas – the brain constructs a scene, and understands where we are with respect to our environment. When any of these brain areas becomes dysrhythmic, our interpretation becomes distorted, for example, we can become hyper- or hyposensitive, as is seen in various symptoms of autism.
With neurofeedback, we can train the brain areas relevant for efficient sensory processing and integration. Personalised Brain Training uses the most advanced qEEG brain map interpretation method to form an individualised training plan. Our neurofeedback method applies the most effective training protocols with an enjoyable feedback process, watching movies of choice.

Sensory processing is a well-researched process that involves many dedicated brain areas, and their interaction to produce an impression of our environment, and how it relates to us. Higher integration of ensuing awareness leads us into the realm of “what is consciousness”:
Science shows that our brain is engaged in a constant process of modelling, or predicting, our environment, both with regard to space and time. It does so on the basis of previous sensory information, as well as recent and consolidated memory. Predictions are then matched with reality, and the process begins again. This is an important distinction from the idea that we are merely reacting to our sensory input. It introduces the theory that we essentially anticipate the next moment, and then update our model of our environment, continually.
Autism can be viewed as an impaired capacity to efficiently engage in this predictive process. The theory easily explains the insistence on sameness and inflexibility with regard to changing routines, embracing novelty, interacting with moving objects, reduced appreciation of humour and even Theory of Mind, which is essentially the creation of a model of another person in one’s own mind. An unpredictable world becomes overwhelming, explaining the fear and anxiety we so often witness with the condition, and resorting to self-stimulation (stimming) is an anxiolytic response. As a result of reduced modelling and predictive capacity, repetition is favoured, and this can turn into a strength as replicative behaviours enhance certain skills or narrow areas of focus.
We can think of autism as brain dysregulation in multiple functional areas. This results in many comorbidities, which we implicitly address with neurofeedback training as part of a holistic approach.
Some of the challenges we have seen to improve with neurofeedback training include:
– lack of bodily awareness, motion control and speech, spatial awareness
– an inability to express, understand and convey emotions and physical needs
– increased frustration at not being understood, whether on a basic survival needs level or in more emotional / intellectual areas
– impulsive aggression, potentially morphing into self-fuelling rage and violent behaviour, sometimes self-directed
– perceived lack of empathy and regard for the needs of others
– generally being ‘misunderstood’, to the detriment being able to fully develop strengths and talents
With neurofeedback training, we can address these ultimately self-harming divergences and bring out the incredible potential in all of us.
Neurofeedback training has been shown to be a safe, feasible, and effective therapy approach to Autism Spectrum Disorder across all ages.
Multiple studies confirm:
– improved cognitive flexibility
– improved facial recognition
– better behaviour, including being less aggressive, more cooperative and better at communication
– improved functional connectivity in the social brain regions.
A 9 point improvement in IQ was reported alongside decreased ASD symptoms including attention, anxiety, aprosodias, social functioning, as well as academic and intellectual functioning.
Sensorimotor behaviour (posturography) improved in children.
Neurofeedback training has proven calming effects.
Research evidence for comorbidities, e.g. ADHD, dyslexia, depression, anxiety, seizures, sleep and behaviour is shown under the relevant tabs below.
Traumatic Brain Injury & Concussion
Traumatic Brain Injury (TBI) is another application of neurofeedback training.
We have found neurofeedback to be highly effective in assisting physical rehabilitation. With a Kaiser Neuromap, we can detect areas of hypometabolism that respond hemodynamically with neurofeedback training. There are neuromarkers for mTBI, as well as Alzheimer’s Disease, though these are non-specific (necessary, not sufficient conditions) and should not be seen as diagnosis. General (rather than focal) lesions in neurodegenerative conditions appear to form first in the corpus callosum, a fibre bundle linking the two brain hemispheres; altered functional connectivity has been visible there on a brain map too, in our experience, at an early stage.
There is evidence that neurofeedback supports myelination, improving the important sheathing of axons, which is a critical part of the physical recovery process.
Pain perception has neural correlates – there are brain areas that govern our attentiveness to the signs our bodies are giving us.
In the first instance, these signs are real messages that something is wrong and needs dealing with. Medical attention should provide solutions to this.
Sometimes, pain perception can become irrational in this context, and with neurofeedback training we can help the brain establish a more reasonable approach to interpreting such stimulus.
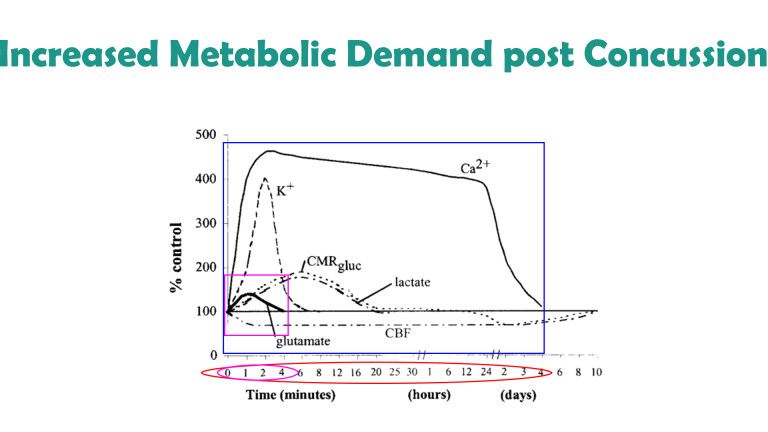
Immediately following concussion / mTBI, there is an increased demand on energy (glutamate) in the brain, at the same time as cerebral blood flow is constrained.
This effect is most pronounced during the first four minutes following impact; other neuromodulatory impairments last for days, and it is estimated that cerebral blood flow is only normalised after around ten days. The blood brain barrier is temporarily disrupted in the first few minutes leading to a complex inflammatory response in the hours and days following injury, and microglia can remain activated for many years.
There are numerous neuromarkers of mTBI, ranging from reduced prefrontal activation to impaired Default Mode Network functionality; while these are non-specific – necessary, but not sufficient conditions – some are highly unusual and show up on a Kaiser Neuromap. With neurofeedback, we can train these, while restoring general functionality of our neural basis of self (the Default Mode Network). We have seen impressive recoveries, both with regard to client feedback and before/after brain maps.
Concussion / mTBI increased the risk of Alzheimer’s Disease by 50% and shares similar mechanisms of promoting tau / amyloid pathology. TBI also increases the risk of Parkinson’s Disease and is capable of producing a prion-like spread of self-seeding proteinopathy. Moderate to severe TBI adds around five years to measured brain age, relative to chronological age.
Trauma, (C-)PTSD
Trauma and abuse leave scars.
When the viability of our existence has been subjected to threat, our behaviour adapts. We become primed for hypervigilance, sensitive to triggers, and our physiology responds accordingly. A heightened sense of awareness now confers safety, and we can even become addicted to this.

Our brain keeps the score: Areas responsible for defence and vigilance are activated, even when there is no objective reason. Sensory stimulus is amplified, and we dedicate value energy resources to the monitoring of others’ intentions. Anxieties are rekindled, and the strain on our system leaves us exhausted while unable to switch off and effectively recuperate. Our focus and productivity drop, as does our self-esteem. We can feel detached from our bodies, dissociating. Our social capacity is impaired.
Neurofeedback helps us break this cycle: we equip the brain to get over it, to get on with it, re-establish our sense of self-worth, and the ability to constructively engage with our environment. We gain a healthy sense of detachment, which allows us to process the past more efficiently and look forward to the future.
With a brain map, we can identify which parts of our system are being particularly stressed. Neurofeedback training helps us bring these brain areas into better alignment.
Typical Symptoms of Trauma and PTSD
The first indication that we are experiencing trauma / PTSD is when we find ourselves not living in the present. Enjoyment of the moment and social interaction is clouded by constant ruminations about the past, and worries about the future. We are unable to ‘let go’, relax, and grasp opportunities as they present themselves in the Now.
We are plagued by intrusive thoughts that bring us back to events in the past, which needn’t even be related to a traumatic event, but which remind us of some inadequacy and amplify our self-doubt. Feelings of shame and guilt come into the picture as well, further eroding our self-confidence. “How can I be happy and enjoy this after what has happened?”. Similarly, our perception of the future is shrouded in worry and fearful anticipation. Uncertainty is our greatest foe, our perception of safety is unhinged by any doubt as to what could happen next.
The absence of a plan becomes a concern, the lack of clarity as to what’s around the corner a burden. Negativity associated with the past deprives us of hope. We are thus unable to see uncharted territories ahead as an opportunity, and much rather dwell on impending threats.
Indeed, our system is primed to protect us, and we are in survival mode. This process becomes self-feeding as we become addicted to the hyper-arousal our sense of fear induces. Our sense of joy and looking forward to fun becomes clouded to the extent we forget and no longer yearn it. Detachment sets in, further isolating us from feelings that previously motivated us. This process can even start slow and subtly, yet the cycle is self-fulfilling and deprives us of the necessary perspective to break and get out.
In Personalised Brain Training, our definition of trauma is wider. We include for example perceived loss of social standing, which can be either the cause or the consequence of a traumatic event or development. The perceived loss of social position results in us feeling judged. We become hypersensitive to how people approach us, talk to us, deal with us.
This is a subjective concept, as it should be, given that trauma should be recognised as an issue of perception by the affected person, rather than a concept being ‘awarded’ by an unrelated party, though external affirmation can help and medical advice should be sought in any event. As humans, social recognition is a critical component of our biological drive to propagate. Attraction relies on this, which ultimately leads to bonding.
Consequently, there are numerous brain areas devoted to, or involved in, the assessment of our position with regard to others. When our self-perception is assailed, or even the viability of our self is questioned, we are naturally shaken. Various brain areas become dysrhythmic. These include areas responsible for our body control and awareness, and many therapies focus on engaging the body and somatosensory system with a view to inducing cerebral changes.
However, this is only a part of the picture – there are many, arguably more powerful neuronal centres in the brain that are affected by trauma, and with a Kaiser Neuromap and Default Network Training (together, Personalised Brain Training), we can assess the issues more accurately, completely and efficiently, as well as then successfully training the brain to overcome trauma and setting ourselves on course for a positive trajectory.
Another consequence of trauma is that we may feel unable to rationally assert a sense of safety. This is different to self-nurture, or an emotional sense of safety. When we are unable to talk ourselves down from a situation we lose the ability to effectively regulate our moods, to switch off when we need to, and ultimately can become excessively paranoid.
There are neural correlates for this behaviour, and we can asses this with a Kaiser Neuromap. Safety and assurance are core needs we are programmed to seek to fulfil. Authority and role models help us in this quest. When we become dysregulated in our ability to self-soothe, we are also compromised in our ability to find paternal guidance. As a result, we tend to over-idolise figures who seemingly exude strength and power, or disobey completely and become unnecessarily rebellious – both immature behaviour patterns. Resetting this balance is crucial to achieving calming, regulated emotions, reduced hypervigilance and controlling impulsiveness. Personalised Brain Training lets us achieve this.
When hypervigilance persists untreated, we face further problems.
Physically, our heart beats faster and harder, more of the time, which is a clear stress on our system.
Mentally, we become prone to developing intrusive thoughts, even when we are able to relax, and more so when we are stressed, where these can take on third-person character, a voice in our head. This can have a destabilising effect, not least because we are now spending energy ‘defeating’ other perspectives we are internally engaged with, and thus distracting us from the ‘now’. Being on hyper-alert can also make us more susceptible to feeling relational to sensory input, in that we feel that everything is directed at us, which can set us up for psychosis.
As we lose our ability to enjoy the moment, our social interactions suffer. Exercising our social brain keeps us alive and forms the basis for sound mental health. Our brains are adaptive, and we need to provide stimulus to maintain connections and sustain flexibility. Isolation deprives us of many necessary exercises. For example, brain areas that deal with face recognition also respond to affective interactions and the ability to discriminate between emotional content of faces. We need to keep training these brain areas through social interaction in order to maintain emotional recognition – it is not a surprise that perpetual mask-wearing heightens our social anxiety (aside from adverse physical effects).
Social recognition, a key component of our biological need to attract and bond, is driven by sensory interpretations. Again, we need to exercise brain areas that contribute to this, including language and speech generation and comprehension, auditory sensitivity, and monitoring rewards for actions, both directly and vicariously. Our mirror neuron system contributes towards learning from others’ mistakes or examples, and consequently the storage of social rules necessary for constructive functioning in a society.
Inclusion is imperative to establishing a healthy self-image or sense of self. This in turn is crucial to forming stable relationships with friends, family and forming healthy alliances necessary for personal and professional progression. When we lose our sense of belonging to a group or cause, we may become unstable in our self-perception and our relationships with others. The effect may snowball into perceptions of abandonment, feelings of emptiness and dissociation; this in turn correlates with mood dysregulation, impulsive and often dangerous behaviours, intrusive thoughts and potential self-harm.
With Personalised Brain Training, we can assess vulnerability to these traits as they manifest in functional brain area dysrhythmia that shows in a Kaiser Neuromap; with Default Network Training, an advanced form of neurofeedback, we can train these brain areas and networks in a holistic manner to help re-establish balance. This enables us to reconnect with our environment and re-enter a positive feedback loop.
Sleep is adversely affected by trauma. First, the mind needs to ‘let go’ in order to enter deeper sleep cycles, which is a challenge for many. Excessive rumination and intrusive thoughts can hinder this, as does the loss of our ability to rationally calm ourselves down. The depth of our sleep is governed by our ability to self-nurture and create an emotional ‘safe space’. Homeostasis during various sleep stages is governed by other parts of our brain, some still involving the cortex. With a Kaiser Neuromap we can detect dysrhythmia in the relevant brain areas and train these accordingly with Default Network Training (together, Personalised Brain Training).
Focus and organisation suffers as a consequence of sleep issues. This time, different brain areas are affected, which we can also train. When we are unable to concentrate and produce our best output, we become demotivated and our mood and sense of self suffer. Again, there are brain areas responsible for these aspects of being, for which we can again detect dysrhythmia and provide neurofeedback training. The process is holistic – many components have to work together effectively for us to function optimally.
Mood regulation suffers when we lose social integration, sleep and focus. Neurofeedback training found to significantly help 80% of people with depression by aiming to restore motivation, improving sleep and focus, and reducing anxiety.
There are numerous potential cortical contributors to depression, and with a brain map we can see vulnerabilities.
Neurofeedback training lets us address these as well as establish a generally improved sense of well-being in a holistic manner. he positive effects of neurofeedback training have been shown to be lasting. Neurofeedback is non-invasive and medication-free.
There are multiple types of anxiety, each correlating with one or more brain areas being dysrhythmic:
- Social anxiety: When we’re in a situation with other people and our understanding of the social dynamics and complexities is overwhelmed.
- Sensory overload: our brain interprets all sensory stimulus as directed to ourselves. We lose the ability to discern what is directed at us, and which matters or interactions are of no concern to us. This sets us up for panic attacks and ultimately psychosis. It also means we become singular in our perspective, unable to take on other points of view
- Loss of narrative: Our episodic understanding of the situation, how we got there and what happens next, is impaired, and we are unsure of where we are and where we’re going. This hyperactivates our amygdala, and the sensation is highly emotional
- Auditory sensitivity: we become prone to overly interpreting the emotional content of words and sounds, creating an air of prickliness and pushing people away without knowing it
- Activation: Our ARAS is responsible for setting the right level of physiological arousal, or wakefulness, for the situation, and to remain stable there. When this is on overdrive, we are pushed further into fight-or-flight mode than necessary, thus heightening sensory sensitivity. Panic attacks are an extreme manifestation.
- Trauma: an inability to self-nurture – creating an emotional safe-space around us – and self-soothe – being able to talk ourselves down rationally from a situation, thus resulting in mood instability. This can also manifest in dissociation and heightened pain perception. We ruminate about the past and worry about the future, instead of being able to enjoy the present.
- Intrusive thoughts: Self-criticism overshadows motivation and confidence, and we become self-aware and distracted by negative thoughts and feelings. Some use acquired habits to distract from this. Our confidence, motivation and social interaction suffer as a result.
The primary issue of trauma affects brain areas that are activated during empathy and forgiveness. With these two qualities impaired, our emotional life suffers, as do our social capacities. With neurofeedback training, we can restore functionality of these brain areas. Another reason this is important is because we do not want to become oppressors ourselves. As we lose our sense of emotional investment in our surroundings, we become careless with regard to others’ feelings and needs.
Implicitly, we are now capable of unintended yet real behaviour patterns that can harm others, as we become deaf to feedback. Not only has trauma affected us, it now makes us perpetrators that pass it on.
Besides reduced social interaction and a less meaningful emotional life that is now more self-centred – and with the wrong type of therapy, becomes self-indulgent and self-perpetuating – we can experience a physical withdrawal from our environment. Dissociation can be momentary and intense, or subtle and ongoing to the extent that we are not even cognisant of it. Either way, our bodies retreat from sensations, analogous to our emotional withdrawal.
Many therapies aim to revive our sense of ownership of our bodies, and thus ultimately our life and future, by training our body awareness in various ways. Realising that our bodies are steered by our mind, specifically our cortex, we can train the relevant brain areas that govern our body perception and movement execution.
Neurofeedback training effectively complements these approaches by directly treating the areas involved in perception and interaction with our surroundings.
One of the first manifestations of trauma is in our bodies. Aside from heightened physiological arousal, a form of paralysis can override our natural motions and postures. Stress, and pain ensue, which can often be felt all around the body. Fibromyalgia is a variant of this phenomenon, as are headaches, chest pains, and chronic fatigue.
There are many techniques for combating this form of physical dissociation. Neurofeedback complements these by training the brain areas that instruct the body to behave in this undesirable way. It is a holistic approach, and we restore overall calming while providing the brain with rational and emotional capacity to overcome its challenges.
Dyslexia
Dyslexia often presents together with ADD/ADHD and other behavioural issues. With a Kaiser Neuromap, we can assess vulnerabilities, and then train these with Personalised Brain Training.
Dyslexia is an impaired ability to understand written and printed words or phrases and affects 10-20% of the population in both males and females. The disorder can result in learning difficulties, poor academic performance, stigmatisation and ensuing behavioural issues.
While often classed as a disability, there are associated strengths: creativity, the ability to solve complex problems, unorthodox approaches to ideas and projects, and a more detached ability to apply logical thinking are some of these. Nonetheless, the condition can impair school and social functioning, slow maturation and significantly affect self-confidence and -esteem.
“Picked up a book and started reading! Unheard of before, I could never get her interested in reading for herself.” – Mother of Anna (9)
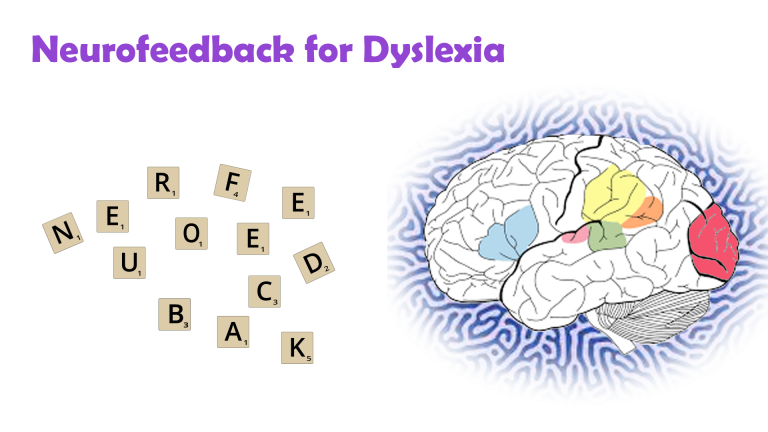
There are neural correlates with dyslexia which we can train with neurofeedback.
Reading and comprehension involves multiple brain areas as well as their seamless communication. We have Wernicke’s area for comprehension, and Broca’s for speech generation. Additionally, there are regions involved in sequencing, visual recognition, focus and attention, and contextualisation or syntax recognition of subject matter along with various memory-related areas.
It is important to note that there are different types of dyslexia. A brain map shows us which brain areas are dysrhythmic.
With neurofeedback, we train brain areas involved in visual and auditory processing; memory; focus and attention; syntax and context; sequencing and organisation. We also train the connections between these areas. The approach is holistic: we work on core networks, and their integration with each other.
Research on Neurofeedback and Dyslexia
Research has shown that neurofeedback training can improve reading ability and phonolocigal awareness deficit in children with reading disabilities, as well as improvements in spelling.
For a summary of 18 neuroscientific research studies on language learning impairment produced until 2015, see here.
Menopause
Menopause can have adverse cognitive and mental health symptoms. This is a particularly difficult time when raising children with strong emotional needs as they enter puberty contemporaneously. Ideally, we would like to be grounded and able to offer support while going through a transformative period ourselves.
Neurofeedback training has been shown to be an effective, non-invasive, medication-free treatment for many mental health issues precipitated or exacerbated by menopause..
It is a complementary therapy and evidence presented is based on general applicability, rather than being menopause-specific.
The menopausal transition is often accompanied by mood, memory and sleep issues.
Managing symptoms becomes important to avoid cumulative effects resulting in cognitive impairments.
Symptoms experienced during menopause include:
– weight gain and body awareness issues
– anxiety
– depression
– sexual dysfunction and impaired sense of self
– sleep disturbance
– brain fog: attention and working memory issues
– vasomotor irregularities: hot flashes, night sweats
Personalised Brain Training aims to restore a healthy sense of self by working on brain areas that are core to our individuality, and addressing areas contributing towards anxiety, mood regulation, sleep, memory and physiological self-regulation.
The process is enjoyable – while watching a movie, we obtain a real-time measurement of a particular brain area’s performance. Feedback is given via small changes in volume, which our preconscious mind understands and uses to adjust it’s behaviour, thus learning to be more efficient. The result is a feeling of calm and self-assurance, with improvements in focus, motivation and sleep. Responsiveness can usually be assessed within a few sessions.
Depression, Bipolar Disorder, Mood Regulation and Motivation
There are numerous contributors to depressive tendencies from a neural perspective. A brain map lets us identify possible cortical contributors, and we can train important neural hubs that affect our ability to regulate mood.
In this sense, neurofeedback is a next-generation treatment for depression. We seek to avoid reliance on medication, especially from an early age.
The effectiveness of neurofeedback training in treating depression is well-documented. Effects have been shown to be strong and lasting. Working on depression helps us re-establish our sense of safety in the world, and often correlates with our ability to fall asleep.
There are multiple contributors to Depression, and neurofeedback has been shown to help with each:
– mood regulation and stability
– motivation and productivity
– sleep and effective recuperation
With Personalised Brain Training we take a holistic approach: Key neural networks responsible for our sense of self, for focus and productivity, and for mood regulation are addressed during neurofeedback training. The process is non-invasive and medication free, as well as enjoyable as we use movies to embed the feedback.
Bipolar disorder affects one in five people with depression. Again, we can address brain areas responsible for maintaining stability, and help calming, particularly important during manic episodes, thus seeking to avoid psychosis. Also, given that more than two-thirds of bipolar disorder sufferers are misdiagnosed initially, identifying the presence of non-specific neuromarkers can aid (but not replace) the diagnosis process.
Examples for the Scientific Basis of Neurofeedback
The US National Library of Medicine records over 140 peer-reviewed research papers on neurofeedback and depression, with a significant recent rise in research attention to this non-invasive, drug-free treatment method. Here are some excerpts of the scientific evidence supporting neurofeedback for depression. Note the diversity of brain areas involved, suggesting that depression need not have a single nor consistent source, and the comorbidities often found:
Dr. Corydon Hammond finds in his 2005 paper, “Neurofeedback Treatment of Depression and Anxiety” that neurofeedback training results in “enduring improvements approximately 80% of the time”, with most perceiving a difference after between three and six sessions; a “very significant improvement” after 10-12 sessions, and more so after over 20 sessions.
Twenty sessions of neurofeedback training led to a significant improvement in sleep, anxiety and depression evaluations. The same disorders plus inattention showed significant improvements when conducting ten or more sessions in a naturalistic setting.
Neurofeedback improved depressive symptoms in Major Depressive Disorder (MDD) patients, with significant decrease in anxiety and clinical illness severity noted as a result of the training. Cognitive depression was reduced here. Anhedonia and comorbid anxiety in MDD were also improved in this recent study. Cognitive impairment during MDD is recognised and neurofeedback treatment advocated. Its effectiveness on a variety of cognitive functions in MDD such as working memory, attention and executive functions is established.
Neurofeedback is recognised as a next-generation treatment for Major Depressive Disorder.
Increased happiness ratings, mood improvements and decrease in anxiety was documented with related increased activity in specific brain areas. Cognitive-affective brain areas as neural targets for treating depression are recognised here, while higher-order visual areas are implicated in this study that recognises that neurofeedback training can reduce depressive symptoms by over 40%. Further success in treating MDD with comorbid anxiety symptoms was documented here, training specific brain areas.
Sub-threshold depression was improved in college students and recommended as an effective new way for college students to improve self-regulation of emotion.
Rumination, a maladaptive emotional-regulation strategy, was found to have a neurological basis that was successfully reduced while ameliorating depression. The tendency to preferentially attend to negative stimuli in the world and negative thoughts in mind during depression was found to be controllable with neurofeedback. Ruminative processes and avoidance when dealing with autobiographical memories were attributed to specific brain areas and recognised as contributing to Major Depressive Disorder, promoting neurofeedback training as a depression treatment. Similar brain areas when trained with neurofeedback resulted in improvements in self-esteem.
Training brain areas responsive to negative stimuli decreased negative cognitive biases in MDD, showing greater decrease in self-reported emotional response to negative scenes and self-descriptive adjectives. Neurofeedback training is also able to improve processing of positive stimuli in MDD patients. Another recent study achieved significant improvements in reducing the severity of depression and rumination in MDD training a different brain area. Lasting effects of reinforcement learning of better brain habits on rehabilitating emotion regulation in depression through neurofeedback were found. Depressive symptoms were alleviated consistently.
The treatment resistance of recurrent depression is linked to rigid negative self-representations during an identity formative period in adolescents, with potential lifetime repercussions. The study finds neurological evidence for which it recommends neurofeedback interventions. Significant and lasting improvements following neurofeedback training were discovered in another study on Treatment Resistant Depression (TRD). Significant reduction in depression symptoms were reported after four neurofeedback sessions in patients showing no response to current pharmacological or psychological therapies for depression.
Post-operative depression and anxiety, pain, difficulties sleeping and attention and memory problems were resolved in 20 neurofeedback sessions. The 45-year old female was able to return to work subsequently. Cancer patients found non-invasive, drug-free neurofeedback to ameliorate pain, fatigue, depression and sleep. Chronic Stroke victims found neurofeedback therapy to reduce anxiety and depression level while improving motor, verbal and cognitive skills.
Opiate addicts treated additionally with neurofeedback showed greater improvement in depression and somatic symptoms, and relief from withdrawal, as did cocaine addicted individuals.
Multiple Sclerosis sufferers saw depression, fatigue and anxiety reduced, and the results were maintained at a 2-month follow-up.
Elderly patients found a significant improvement of their depression condition following neurofeedback treatment.
Surgery Residents with burnout and depression saw a return to a more efficient neural network following neurofeedback training.
Neurofeedback has been shown to improve sleep quality and sleep onset as early as 1982, with substantially more research interest confirming this in recent years, also in relation with pain and seizures.
Neurofeedback was shown to additionally benefit patients undergoing Cognitive Behavioural Therapy.
Motor Issues, Dyspraxia, Tics, Stutter, Tourette's
Our brain controls our movements. Functional connectivity dysregulation in autism can affect many of the brain areas involved in planning and executing motor actions. With neurofeedback, we can train these areas to improve symptoms in an evidence-based manner.
There are various cortical, and sub-cortical brain areas involved in motor coordination. With neurofeedback, we are training the cortex. Many cortical areas have deep connections to the basal ganglia and cerebellum, and it appears that we are training these deeper structures implicitly.
In our experience, the following issues can resolve with neurofeedback training:
– motor issues, such as dyspraxia and lack of coordination
– stutter and speech production
– facial tics
– uncontrolled, compulsive movements and actions.

Before and after brain maps corroborate these findings; research has so far focused on neuromarkers for these phenomena, and suggest neurotherapy as an adjunct to traditional therapies.
Tourette’s Syndrome can involve many of the above issues, as well as lack of executive control, again an aspect we have seen improve substantially with neurofeedback training.
PoTS - Postural Tachycardia Syndrome
Postural Tachycardia Syndrome (PoTS) was first described in the 1940s, refined in 1993 and finally received a specific diagnostic code in October 2022. It is characterised by exercise intolerance and near syncope upon standing upright, elevated pulse (tachycardia) by 30-40bpm within 10 minutes of standing up, fatigue, anxiety and light-headedness. Often misdiagnosed as chronic anxiety or panic disorder, the group of symptoms comprised by PoTS has a biomarker and increasingly considered an autoimmune disorder, rather than only autonomic nervous system dysfunction. Specifically, increased levels of cytokines and chemokines characteristic of an innate immune condition were found, similar to autoimmune diseases like multiple sclerosis, psoriasis, type-1 diabetes, rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
The condition affects females five times more frequently than males, mainly between 15-25 years of age, with over one million affected in the US alone. PoTS symptoms can persist for years, though half of patients find that orthostatic symptoms and functional impairment subside within five years, and of thost most within 1-2 years. It is estimated that 2-14% of Covid sufferers go on to develop PoTS, while 30% of long Covid patients, especially women, meet the diagnostic criteria.
A client presenting with PoTS like symptoms, recovered within three months of starting neurofeedback training, to the extent that the tachycardia was fully under control and anxieties had subsided substantially. Clinical studies will have to prove correlation. Notably, physical symptoms became manageable, from being previously incapacitating, in a relatively short period of time. This result is encouraging, especially with regard to the speed and extent of recovery, and neurofeedback has been shown to be effective for anxiety. Also, in this person, other neurological issues could be detected with qEEG.
Schizophrenia
Schizophrenia comprises a wide range of thought disorders, which ultimately affect an individual’s ability to share a reality with others. Causes can be trauma, emotional or physical; drug use; stress; genetics.
With neurofeedback training we aim to restore a healthy sense of self; flexibilise the social brain; and ameliorate comorbidities such as intrusive thoughts, mood disorders, focus and attention issues, paranoia and anxieties; and psychosis.
Neurofeedback training can improve functional connectivity and strengthen white matter tracts, both of which are impaired in Schizophrenia.
Each person is different: with a Kaiser Neuromap we assess individual vulnerabilities and train these with neurofeedback. Personalised Brain Training enables the person to unfold their genius in a socially reciprocal manner.
Neurofeedback is medication-free, non-invasive and evidence-based.
While there are certain commonalities between sufferers of schizophrenia, no two brains are the same. On the basis of a brain map we can identify particular vulnerabilities and work on these specifically.
Neurofeedback training can help restore the integrity of the Default Mode Network, the neural basis for ‘self’, as well as switching between self-referential states and active modes (the Central Executive and the Salience Networks).
Emotional self-regulation can be improved and anxiety, depression, sleep and focus issues alleviated.
Neurofeedback can calm the brain and help manage the ‘Voices’, as well as other regions prone to over-priming external agency. Significant reduction in Auditory Verbal Hallucinations (AVH) has been achieved with neurofeedback training.
Psychosis is a state that can occur, and recur, in persons diagnosed with Schizophrenia, Bipolar Disorder, Trauma and neurodegenerative conditions. Note however that it is not a necessary condition for any of these.
Daniel Webster of Neurofeedback London-Brighton has extensive experience working with Schizophrenia patients. Research and experience have shown effectiveness of neurofeedback training for Schizophrenia and its various comorbidities (see other tabs)
Seizures and Epilepsy
One of the first discoveries made in the exploration of EEG, fifty years ago in 1972, was the ability to improve seizure resistance through neurofeedback.
An analysis of studies indicated that 82% of subjects demonstrated significant (more than 30%) seizure reduction, with an average value of 50%.
A 2009 review of studies established that EEG operant conditioning was found to produce a significant reduction on seizure frequency.
Barry Sterman was able to cure a 23-year old female epileptic from seizures using his SMR-biofeedback training over the course of two-and-a-half years.
Another pioneer of the field, Joel Lubar, reached similar results.
In our experience, neurofeedback has improved seizure resistant in many cases, and has always been beneficial in the treatment of secondary mental health effects. Medical attention should always be sought, and sources can be diverse and elusive.
Self-Harm
Impulsive aggression can become self-directed at times. This irrational urge is often triggered when an autistic child doesn’t get what they want, or feels misunderstood and frustrated. Self harm can also take the form of resignation, accepting less than one’s worth, and thus denying oneself recognition and opportunity.
Neurofeedback calms the mind and we can address brain areas contributing to self-harming ideation and intrusive thoughts.
We look to improve sense of self, reduce anxieties and strengthen inhibition levels while reducing self-directed impulsive aggression.
‘Self-harm’ can take many forms, and beyond physical manifestations (e.g. cutting, suicidal thought or even action) it can be more subtle:
– Accepting less than what we’re worth, overly and unnecessarily acquiescing to the perceived demands of others when not at all in our own self-interest, self-deprecation
– an inability to defend one’s own stance and needs are often overlooked and can be very harmful to a person’s development, especially when repeated and consolidated into a character trait.
With a Kaiser Neuromap we can detect vulnerability to such behaviour, including suicidal tendencies or ideation.
This is not diagnosis and it is non-specific in that dysrhythmia of the brain area(s) responsible for this is a necessary, but not sufficient condition. Nevertheless, it is a worthwhile finding that can help prevent worse outcomes by prompting awareness and intervention.
With neurofeedback training, we have helped self-harming adolescents transition from ‘cutting’ and dissociation to becoming engaged young individuals who are able to stand their ground, maturely deal with setbacks and embrace the sense of being part of a community.
Neurofeedback is a complementary therapy and medical attention should be sought in cases of self-harm.
Sleep
Sleep is where we recover – physically, mentally, emotionally.
It is a complex process whereby the brain enters different behaviour patterns in various stages. Slow wave sleep is where our body recovers; REM sleep is where we digest the day’s experiences, consolidate what we’ve learned and let our brain process memories and impressions.
Ideally, we would like to be able to switch off once comfortable, enter a deep sleep and wake up restored and energetic. If our sleep suffers, so do our concentration, productivity, physical abilities and emotional flexibility.
Neurofeedback has been shown to improve sleep quality and sleep onset as early as 1982, with substantially more research interest confirming this in recent years, also in relation with pain and seizures.

"I felt so calm last night! And slept like there were magnets between me and the bed. 10 hours straight."
"Slept like a log."
"Since I started neurofeedback training, my dreams have come back!"
Client testimony.
Что такое аутизм?
Аутизм — это расстройство спектра, характеризующееся проблемами социальной интеграции и задержкой развития, которая может быть как физической, так и эмоциональной. В частности, мы можем выявить и обучить уязвимости в моделях поведения:
– сенсорная интеграция: чувствительность к звуку, свету, вкусу и осязанию, координация движений; баланс, телесное и пространственное осознание; понимание и производство речи
– социальное функционирование: социальные сигналы, очередь, теория разума, сотрудничество с другими, социальные правила и границы, различие между собой и другими.
– саморегуляция: контроль настроения и импульсивности, импульсивная агрессия и ярость, страх и тревога, способность к самоуспокоению/самовоспитанию, повторяющееся ограничительное поведение.
– когнитивная гибкость: моделирование намерений других; прогнозирование движений, поведения и результатов; обновление моделей и прогнозов на основе наблюдений; гибкая и просоциальная корректировка поведения.
Результатом обучения нейробиоуправлению является более спокойный, лучше интегрированный ребенок или взрослый, поскольку мы даем им возможность максимизировать свой истинный социальный и продуктивный потенциал.
Социальное развитие при аутизме
Социальное развитие людей с РАС может быть нарушено следующим образом:
– недостаточно развитая Теория Разума, то есть приписывание намерений/эмоций/перспектив других, умозаключение психических состояний, моделирование поведения других/предвидение этого
– отсутствие дифференциации себя/других
– социальные тревоги, непонимание социальной сложности, избегание социальных контактов и практики социальных навыков.
– непонимание социальных границ и правил, что приводит к, казалось бы, неадекватному поведению.
– очевидная нечувствительность к социальным эмоциям и, следовательно, отсутствие существенного (невербального) контекста.
– неспособность отразить и установить контакт
– усталость, несосредоточенность или иное отсутствие необходимой мотивации для поддержания социальных взаимодействий, что приводит к образованию петли отрицательной обратной связи.
Вышеупомянутые проблемы развития могут привести к отсутствию практики и осознания ситуаций, требующих все больше усилий и ценных энергетических ресурсов. Недоразвитое понимание социальных границ и правил, тревоги, отсутствие мотивации и сосредоточенности, а также чувство повторяющейся изоляции еще больше усугубляют недостаток уверенности и могут еще больше лишить человека возможности учиться и получать положительное подкрепление.
Речь и язык являются важнейшими компонентами личного взаимодействия, обмена эмоциями и точками зрения, а также тренировки значительной части наших нейронных сетей. Возникает петля отрицательной обратной связи, поскольку личное развитие (и уверенность) является результатом нашего взаимодействия с другими людьми, что, в свою очередь, зависит от физической способности к общению, ключевыми компонентами которой являются речь и язык (вербальный и невербальный). [Тем не менее, простое физическое присутствие может быть воспринято и многое передать]
Тенденции и распространенность аутизма

Теоретически аутизм можно достоверно диагностировать к 2 годам, хотя у большинства из них диагноз не диагностируется до 4 лет, а из-за задержек, связанных с пандемией, в последние годы этот показатель увеличился до 8 лет. Мальчикам в четыре раза чаще ставят диагноз аутизм, чем девочкам, и существуют значительные различия по этническому признаку.
Тревожной тенденцией является значительное увеличение общих показателей: в настоящее время аутизм диагностирован у одного из 36 детей в США, то есть в 2020 году по сравнению с одним из 44 в 2018 году по сравнению с одним из 150 в 2000 году. В Великобритании общая распространенность этого заболевания оценивается в 1/100, или около 700 000 больных в целом. По данным Университета Ньюкасла, он составляет 2,8% среди мальчиков (1/36) и 0,65% среди девочек (1/150). Медицинский журнал Lancet сообщает о частоте заболеваемости 1/250 среди детей в возрасте 5–9 лет, 1/4000 среди людей 20–49 лет и 1/18000 среди людей старше 50 лет.
С 2020 года количество заявок PIP в Великобритании по поводу расстройств аутистического спектра увеличилось с примерно 450 в месяц до более 2000 в месяц.
Поиск причин привел к серьезным дебатам и противоречиям. Однако несомненно то, что раннее вмешательство может существенно повлиять на результаты в отношении развития, качества жизни, а также потребностей в уходе и поддержке.
Карты мозга и нейробиоуправление не позволяют поставить диагноз. Однако мы можем определить уязвимость к симптомам и их корковый источник и работать над ними посредством тренировки. Мы можем сделать это в любой момент жизни человека и не сдерживаемся противоречиями между внезапным появлением симптомов и диагностическими критериями (например, PANS/PANDAS).
Существует несколько причин, по которым нельзя ставить диагноз РАС:
– воспринимаемая социальная стигма – игнорирование проблемы
– чувство, что отказ от навешивания ярлыков на ребенка помогает ему лучше развиваться
– чувство беспомощности; поскольку это заболевание сохраняется на всю жизнь и не имеет очевидного лечения, надежды, похоже, нет.
– отсутствие поддержки на местах
– время, необходимое для получения диагноза и стоимость этой процедуры в частном порядке
Улучшение информационно-пропагандистской деятельности может помочь решить все эти проблемы и обеспечить персонализированный и адекватный уход для всех.
Формальная диагностика может дать следующие преимущества:
– самопринятие: после постоянных личных трудностей, снижение самообвинения
– принятие другими
– расширенная поддержка, как в школе, так и на рабочем месте
– расширение прав в соответствии с Законами о равенстве и психическом здоровье.
– доступ к льготам и другим условиям ухода
– доступ к долгосрочному уходу
– доступ к образовательным ресурсам (SEN)
Autism Diagnosis Criteria per DSM-5
Autism is diagnosed as follows by the DSM-5:
A: Persistent deficits in social communication and social interaction across multiple contexts
B: Restricted, repetitive patterns of behaviour, interests, or activities
C: Symptoms must be present in the early developmental period
D: Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning
E: These disturbances are not better explained by intellectual disability or global devlopmental delay
Severity of the above symptoms can vary, hence the notion of a “spectrum disorder”. It is graded in three levels, commensurate to the level of support required.
Further specifications include: intellectual impairment; language impairment; other neurodevelopmental, mental or behavioural disorder; catatonia; association with a known medical or genetic condition or environmental factor.
The Autism "Triad"
The triad of impairments is as follows, with some overlap between each:
– Communication: difficulty in expressing needs, emotions, feelings; impaired language development; understanding prosody; rigid speech patterns
– Interaction: issues with personal and social boundaries; self/other differentation, turn-taking; verbal / non-verbal cues; making eye contact; developing and sustaining relationships
– Social Imagination / Restricted and repetitive behaviours: self-stimulating (“stimming”), repetitive behaviours to the exclusion of others and lacking play, exploration and imagination; ‘excessive’ focus on particular themes/topics, inability to take on different perspectives or others’ emotional states and intentions
Brain Differences in Autism
There are some detectable brain differences in people with ASD, including structure and connectivity. These include:
– Brain volume trajectory: ASD brain volume growth appears accelerated, particularly in the frontal and temporal lobes, in early children around two to four years of age. Adults on the other hand appear to show decreased volume or no difference, and it is thought that growth is arrested after around 10-15 years or age. Led by an accelerated expansion of the cortical surface before the age of two, without concomitant increase in cortical thickness, this expansion of gray matter appears linked to lower maturation of the cortical white matter, giving rise to atypical connections.
– Specific cortical regions have been suggested as being responsible for the various symptoms exhibited as they relate to language, social attention and behaviours, and repetitive and restricted behaviour, while accepting their heterogeneity.
No two brains are are the same, and this holds true for ASD in particular. A qEEG-brain map can show areas of dysrhythmia that could benefit form training in a personalised approach
– Enlarged amygdala in autism, specifically a subregion responsive to both salient stimuli and threats. The amygdala is a key subcortical element of the limbic system with strong links to certain cortical sites. We can train these cortical sites with neurofeedback.
– Grey and white matter volumes as well as gyrification in various brain areas are different in autism, including those involved in face and object recognition; intention of others; spacial awareness; internal organisation; language and expression of emotion.
A brain map can help personalise the neurofeedback training. With Neurofeedback, we can also train the white matter tracts.
Sensory processing and integration issues arise from dyrhythmia, or immaturity, of specific brain regions. Differences can include:
Auditory – discerning between background noise and relevant sounds; distraught or comforted by loud noise; attributing emotional content to sounds (or not); immersion in or ignorance of soundscape (comfort)
Visual – foveal vs. peripheral sensitivity variations and focus; colour perception and attributable comfort / pleasure / distraction; depth rendering; movement cognition; light intensity; scene construction / disjointment; temporal prediction error in moving scene
Tactile – touch sensitivity; association of pleasure with touch; pain threshold (harm alertness); predictability of touch, e.g. randomness of water flow / washing
Olfactory – general sensitivity; extreme association of reward / disgust with smell; distinction and its subconscious impact on social affinity, reward assessment and even dopaminergic (motivational) effects
Gustatory – sensitivity to taste and texture (spicy vs. bland), effect on food intake, extremes e.g. pica (craving non-food ‘taste’); strong links to olfaction and visual appearance. Dietary preferences can be guided by gustatory, visual, olfactory and tactilesensations, as well as their combinations / interplay; rewards in one sensory domain can help overcome aversion triggered in another; e.g. finger food arranged in familiar patterns can help overcome a dislike for the food-type (e.g. vegetables) in question.
The vestibular system helps us detect the position and movement of our head in space, and thus contributes to coordination of movements and posture, including our sense of balance. Hyper- or hypo-sensitivity in this system results in lack of balance, or the need/desire to stimulate it by creating movement (e.g. spinning, hyperactivity).
Proprioception is our sense of where we (our body) are in relation to other objects, space in general, and parts of our body. Hyper- and hypo-sensitivity results in clumsiness, misjudgments, invasion of personal space, pressure regulation and possibly writing; and stimulus-seeking, excessive movement and contact, and the application of weighted clothing, respectively.
Neurofeedback for Autism
With neurofeedback training, we can address the following manifestations of autism as there are specific brain areas responsible for each of the following:
– sensory processing and integration: visual, auditory, tactile, olfactory, gustatory
– sequencing and planning of actions
– motivation and mood control
– awareness of surroundings and consequences of actions
– fear, anxiety, dissociation and detachment
– impulsive aggression and rage
– self/other differentiation
– verbal and non-verbal communication; speech and language
– auditory hypersensitivity
– rigidity of thought and expectation, inflexibility
– repetitive restrictive behaviour
– vulnerability caused by excessive recruitability (“being too nice”)
– motor function, mobility and coordination
– empathy and emotional understanding of self and others
– sense of self
– social boundaries
– dissociation, detachment and the feeling of needing to mask behaviour
– focus, concentration and organisation
– sleep: onset and quality
Neurofeedback for autism is a non-invasive, medication-free complementary therapy. It is safe, evidence-based and effective. Moreover, it is an enjoyable process that simply involves watching movies or YouTube clips – feedback to our brain is merely audio-visual, as small changes in volume and picture size provide the brain with enough information to mature its behaviour patterns.
Personalised Brain Training respects neurodiversity. With a brain map, we identify areas of cortical immaturity and train these. As such, we can improve group-minded thinking and the ability to thrive while preserving individuality.
Sensory processing is a well-researched process that involves many dedicated brain areas, and their interaction to produce an impression of our environment, and how it relates to us. Higher integration of ensuing awareness leads us into the realm of “what is consciousness”:
Science shows that our brain is engaged in a constant process of modelling, or predicting, our environment, both with regard to space and time. It does so on the basis of previous sensory information, as well as recent and consolidated memory. Predictions are then matched with reality, and the process begins again. This is an important distinction from the idea that we are merely reacting to our sensory input. It introduces the theory that we essentially anticipate the next moment, and then update our model of our environment, continually.
Autism can be viewed as an impaired capacity to efficiently engage in this predictive process. The theory easily explains the insistence on sameness and inflexibility with regard to changing routines, embracing novelty, interacting with moving objects, reduced appreciation of humour and even Theory of Mind, which is essentially the creation of a model of another person in one’s own mind. An unpredictable world becomes overwhelming, explaining the fear and anxiety we so often witness with the condition, and resorting to self-stimulation (stimming) is an anxiolytic response. As a result of reduced modelling and predictive capacity, repetition is favoured, and this can turn into a strength as replicative behaviours enhance certain skills or narrow areas of focus.
Again, there are neural correlates for this. Our Default Mode Network (DMN) is a set of brain areas that constitute our neural basis of self, and is preferentially activated when we are engaged in self-reflection and imagination. In awake state, we oscillate between activation of our DMN and our Task Positive Network (TPN). In a mentally healthy, neurotypical person, the correlation between their respective activation is anti- or counter-cyclical, meaning that when one is active, the other is not, and vice versa. In ASD, this segregation is impaired, as well as the within-network integrity of the DMN. This is a connectivity issue rather than lack of tissue – the ASD brain enjoys a faster growth during its first year, and results in a 2-4 year old ASD brain being no different from a neurotypical adolescent or adult in the majority of cases.
Traditionally, we would think of our TPN as being reliant on sensory input. However, REM sleep is an example of intense DMN DEactivation, and hence TPN activation, yet in this stage we are not actually taking in sensory input. This shows us that our brain generates its own interpretation of reality, and in the extreme (sleep) can do so without resorting to cross-checking with sensory input. The fact that REM sleep is our prevalent condition from at least week 23 / 3rd trimester through our first year of life is testament that consciousness does not explicitly depend on external input. Our perception of reality is self-generated, almost like a simulation. This predictive capacity is likely impaired in autism.
With neurofeedback, we can train our Default Mode Network, and its connectivity with our sensory systems. This leads to improved feeling of ‘groundedness’, sensory integration and synchrony with our environment. When we train sensory processing sites, we are strengthening our Task Positive Network. There are training protocols that reward efficient transition, and neurofeedback training on the whole improves our predictive capacity and hence general flexibility and sensory integration.
Autism Legislation and Advocacy
UK Mental Health and Equality Legislation
Current UK legislation and guidance with regard to autism is as follows; the acts outlined put responsibility on public services in a forward-looking, anticipatory manner, and provide resources to accompany them through their life to avoid harm and further self-empowerment, thus preserving dignity and life itself.
2009 Autism Act – requires the government to introduce and keep under review an adult autism strategy, implemented partially by local authorities and the NHS; this resulted for example in 93% of areas in England now having an adult diagnostic service, with over 50% not having one before 2009
2022 Health and Care Act – introduced a legal requirement for all health and social care services registered with the CQC to provide employees with training on autism and leaning disabilities (“Oliver McGowan Training”, after a Bristol boywho died age 18 in 2016 who was given anti-psychotic medication Olanzapine and suffered simple partial seizures while in care and ultimately died of pneumonia and hypoxic brain injury, caused by Neuroleptic Malignant Syndrome (NMS), an adverse effect of Olanzapine, though the coroner concluded that Olanzapine had been properly prescribed; the family believe that the hospital did not meet Oliver’s needs on arrival through chemical restraint, thereby increasing his distress, in contrast to the coroner finding the care which led to his death was “appropriate”)
Mental Capacity Act 2005 – provides five principles for the protection and empowerment of people who may lack the mental capacity to make their own decisions about their care and treatment over 16 years of age; these include a presumption of capacity; support for making their own decisions; increased flexibility of perspective on “unwise decisions”; a duty to act in their best interests; and a requirement to provide the least interference with the person’s rights and freedoms of actions, assessing particular circumstances.
2010 Equality Act – places a requirement on UK public services to anticipate and prevent discrimination against people with disabilities, including people with a learning disability, autism, or both
The 2010 Equality Act also pertains to the avoidance of discrimination in schools and places of higher education; SEN (Special Education Needs) support extends to progress checks and assessments to affected children under 5; special learning programmes, extra help from assistants and physical / personal care to the age of 15.
Under the Mental Health Act (1983, updated 2007), an Independent Mental Health Advocate is to be supplied to anyone detained under this Act, and they have a right to a Care Act advocate, supporting people with issues relating to their mental health care and treatment.
Promoting the Rights of Persons with ASD
Examples how the rights of individuals with autism can be promoted:
– knowing and understanding existing legislation and guidance relating to autism, mental health, disability and equal rights, and acting on these, such as implementing person-centred care
– taking a critical approach to media reports on autistic persons, understanding generalisations and pointing these out to others, including directly back at the press, as well as around others who might not be aware of this
– challenging discrimination and taking a pro-active stance in implementing the guidance and legislation, as this is ‘alive’ and depends on general awareness and accurate and appropriate actions
– enabling the person with ASD to be directly involved in conversations and decisions pertaining to them, and helping to avoid unnecessary intermediation
– supporting advocacy groups and promoting further causes that keep the momentum going, as previous milestone legislations have shown.
Every person on the autism spectrum is different, with regard to abilities, needs and goals, so to comply with the person-centred approach (and the Mental Capacity Act), as well as the general goal of compassionate, human interaction, a carer needs to understand the individual’s point in their path, how far they’ve come, which goals have been set by them and their team, and what position they are in at the present time to pursue that path. Achieving one’s potential is an important part of developing a healthy sense of self and having a good quality of life, while also providing a positive feedback loop that can help mitigate many other challenges they are facing as a result of the comorbidities of ASD, both mental and physical.
Person-Centred Support for Autism
Person-centred support focuses on care on the needs of individuals, ensuring that peoples’ individual preferences, needs and values guide clinical decisions, and providing care that is responsive, tailored and respectful to them. It was developed in partnership with Skills for Health and Skills for Care, and sets a framework to share best practices that can be implemented by various care segment, such as health, social, housing and local authorities. It is a framework launched in 2018 involving engagement, relationship building skills, delivery of training, education and learning opportunities, and identifies enablers to further this cause.
It is important to treat an ASD person as an individual because:
– everyone deserves to be treated with dignity and respect, and that crucially involves recognising their individuality, with respect to values, needs, goals and care
– people with ASD are, as the name says, on a spectrum, and therefore exhibit individually different needs and challenges. These can range from intellectual, social, communication, physical and emotional, and each person’s manifestation of their blanket “ASD” diagnosis is different.
This also ties in with the person-centred approach described above, with the goal of preserving their dignity on a human level and compliance with the various legislations also described above.
Compassion & Non-Judgment
Some examples of providing support that is compassionate, that is, maximises emotional support in a dignified and constructive way, are active listening, respecting personal boundaries, applying interpersonal techniques such as sitting next to someone who avoids eye contact, instilling hope, having appropriate humour, being optimistic, not getting demoralised, being creative, and generally appreciating someone as equal and human.
Being non-judgmental in one’s approach to care and support involves seeing the other person as equal and human, having a respectful attitude without sense of hierarchy due to perceived abilities; seeing more in the person than their current state might suggest and bringing out the best / maximising their potential; and respecting choices that might appear “unwise”.
Managing Behaviour in Autism: Strategies
Certain behaviours might be responses to a form of sensory overload, and not obvious to spot / make sense of until better empathising or getting to know the individual and assessing the context in which they resort to the behaviour in question. They might be self-protecting, or conditioned into achieving something this way when there are other alternatives that can be taught.
Proactive strategies are pre-emptive, and so applicable when a situation is predictable or known; this can help reduce sensory overload, prevent undesirable consequences and condition positive responses; it may also not work when conditions change surprisingly, and it doesn’t necessarily teach flexibility or adaptation, as well as being possibly over-protective and risk-aversive.
Reactive strategies are generally de-escalating and necessary to avoid harm/self-harm, but as a result of being unforeseen, they might be sub-optimal, not teaching the right behaviour and can be seen as unpredictable and hence hostile by the ASD individual.
Approaches to support positive behaviour are positive reinforcement (operant conditioning); generally rewarding self-initiated, constructive actions; creating environments and subtle (fading) prompts conducive to such behaviour; generally explaining positive and negative behaviour; abstracting this concept gradually to induce internalisation of a thought construct that encourages self-derived positive behaviour; doing so in the context of practical, novel situations to stimulate flexibility and creativity
Communication issues can cause isolation of self and feelings of hostility / misunderstanding by others.
Social skills can impact perceived empathy and further exclusion.
Repetitive, restricted behaviour and likewise result in exclusion and self-absorbtion.
Behavioural challenges can cause harm to others and self.
Generally unpredictable and wrongly interpreted actions can increase stigma and discrimination.
Rule and process adherence can preclude novel experiences for self, and increase burden on carers.
Distraction from the triggering situation; substitution with something enjoyable; positive reinforcement through a compassionate and insightful approach; providing a safe and stable environment, which can often be induced by the presence of someone they trust
Providing respite to be able to regain perspective, and hope; showing empathy and compassion towards them; joining groups with other parents to share experiences and reduce feelings of guilt, stigma and isolation; keeping a temporal perspective by keeping a diary and noting achievements and improvements.
Autism in the Workplace
Rights of ASD individuals with regard to accessing services and facilities have been established through various legislations already outlined above, and repeated here:
Autism Act 2009: specifically requires local authority and NHS to provide access to ASD individuals
Equality Act 2010: prohibits discrimination in such services and facilities
Special Educational Needs and Disability Act 2001: protects rights of students with disabilities
Mental Capacity Act 2005: upholds rights of individuals with limited decision making capacity to make decisions in their best interest / self-determination
People with ASD can be at a disadvantage in competitive workplace environments due to:
– lack of self-confidence and assurance in their relevant skills
– inflexibility when assessing requirements e.g. in ads regarding their suitability
– general and intrinsic discrimination, real and perceived
– difficulty in managing the interview process regarding personal interaction
– general feeling of overwhelm, lack of obvious precedents and role models, paucity of mentors and support while in the job and with regard to creative career management
– not being able to realise transferability of their skills and underestimating their ability to adjust and adapt
– general lack of encouragement due to labelling and stereotyping
We can provide support by:
– finding suitable courses and training events
– presenting these with the goal of enabling the person to make their own decisions (‘coming from them’)
– researching the providers, meeting the teachers, preparing them in advance to enable them to establish quick rapport
– encouragement and promise of reward for attendance
– ensuring attendance
– collecting feedback from provider and teachers
– making sure there are lines of communication at all times and the person doesn’t feel abandoned
– ensuring safe return
– finding appropriate and interesting activities
– conveying these while respecting choice and self-determination
– making transport and attendance as easy as possible
– ensuring attendance
– setting objectives and understanding of the growth opportunity
– positive reinforcement of independence
– liaising with the employer, preparing them for any perceived peculiarities, adjusting the work environment per above
– facilitate initial and repeat attendance logistically
– providing continued encouragement, dwelling on positives and progress, addressing concerns, conflicts and issues and helping resolve these proactively with the employer
– managing the induction process (‘first impressions count’, on both sides)
– general preparation for the ‘unknown’ and reassurance of continued support
– continued encouragement and workplace liaison as above
– communication and management of any problems, issues and difficulties
– ensuring a support environment at work, including HR, mentors, introduction to other employees
– manage the review process, ensure communication is constructive and supportive
– ensure fairness and maximise potential with regard to career prospects
– provide support in the event of challenges, failures (real and perceived), and interpersonal relationships at work
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.
Brain Maps and Personalised Brain Training Explained
Personalised Brain Training with Neurofeedback
Neurofeedback lets us train dysrythmic brain areas. With sensors comfortably fitted to the brain areas we want to train, we detect brainwave patterns real-time while watching a movie. When these patterns are inefficient, the volume drops momentarily. This is the feedback we are giving our brain, short and instantaneously.
The brain area we are training recognises this – while our conscious mind is focussed on the movie – and adjusts its behaviour to restore the normal volume. With repetition, throughout a session, learning occurs.
Meanwhile our conscious mind is solely focussed on the movie; the training process is passive in this sense.
The drop in volume is subtle, so we continue to understand the flow of the movie. No current or electrical stimulation is fed to the brain; sensors simply read brainwaves and the feedback is purely audio-visual.
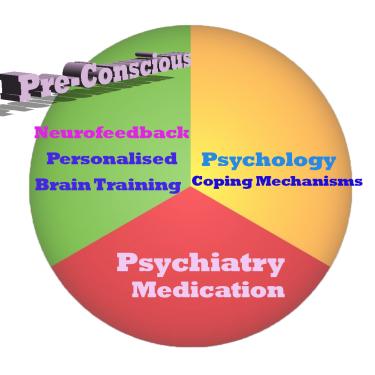
Neurofeedback trains our Pre-Conscious Mind
Rather than engaging the conscious mind, which slows us down, we are training preconscious processes.
This equips us with the ability to live in the moment and attain our potential (if we have to resort to conscious control, we are not living in the moment).
We take a holistic approach to healthy brain self-regulation, rather than categorisation or diagnosis.
Personalised Brain Training is an advanced qEEG brain map-based approach to neurofeedback training developed by the founders of the field. Taking Othmer Method / ILF training methods further, it employs Default Network Training protocols as developed by David Kaiser.
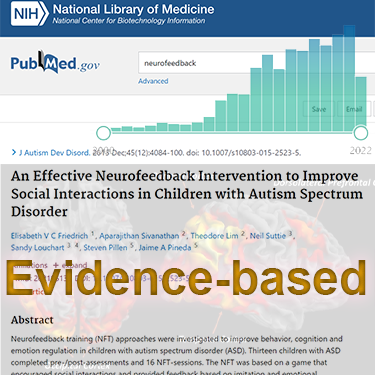
Neurofeedback is Evidence-based
Neurofeedback training is an evidence-based complementary therapy. Its efficacy was first demonstrated some 50 years ago, and with advances in technology, training protocols have become more efficient and the feedback method – watching movies – thoroughly enjoyable.
Neurofeedback is evidence-based. It’s first application was discovered in 1971 when it was used to resolve intractable epilepsy.
There are over 2,000 peer-reviewed research reports on PubMed demonstrating efficacy across a number of pathologies.
In the US, it is an accepted complementary treatment for many challenges.
Neurofeedback is a form of complementary therapy and should not be seen as a replacement for conventional medicine. qEEG brain map-based neurofeedback training takes a more holistic approach to brain functioning, rather than just focusing on medical symptoms. It is not intended as a form of diagnosis nor medical intervention nor medical advice per the disclaimer.